C. diff Symptom Checker
Check Your Symptoms
If you're taking clindamycin or have finished a course in the last 12 weeks, monitor these symptoms. Early detection is critical.
Clindamycin is a powerful antibiotic used for serious infections like skin abscesses, dental infections, and some types of pneumonia. But here’s the catch: it’s one of the riskiest antibiotics out there when it comes to triggering a dangerous gut infection called C. difficile. You might not think twice about taking it-especially if you’re allergic to penicillin-but even one dose can set off a chain reaction in your gut that leads to severe diarrhea, hospitalization, or worse. If you’re on clindamycin or just finished a course, you need to know the warning signs and when to act fast.
Why Clindamycin Is So Risky
Not all antibiotics are created equal when it comes to gut damage. Clindamycin doesn’t just kill the bad bacteria-it wipes out the good ones too. It targets gram-positive bacteria, which includes most of the helpful microbes that keep your gut balanced. When those good bacteria disappear, Clostridioides difficile (C. diff) takes over. This germ doesn’t normally cause harm, but when the gut environment is empty, it multiplies fast and releases toxins that eat away at your colon lining. Studies show clindamycin carries the highest risk of causing C. diff infection among all common antibiotics. A 2019 analysis of over 150,000 patients found clindamycin was linked to significantly more cases than even broad-spectrum drugs like fluoroquinolones or cephalosporins. The reason? It stays in your digestive tract longer than most antibiotics, giving C. diff more time to grow. Even a single dose before a dental procedure has been linked to cases of C. diff. The CDC calls C. diff an "urgent threat," and for good reason. In the U.S., nearly half a million cases happen every year. About one in five of those cases start in the community-not the hospital-often after someone takes clindamycin for a tooth infection or a skin rash.When Does C. diff Show Up?
Most people assume diarrhea during or right after antibiotics is normal. But C. diff doesn’t always hit fast. The average time from starting clindamycin to symptoms is 5 to 10 days. But it can show up as early as day one-or as late as 12 weeks after you stop taking it. That’s why so many people miss the connection. Data from the University of Iowa shows that:- 22% of cases happen while still on clindamycin
- 46% occur within one week of finishing the course
- 68% appear within 14 days of starting the drug
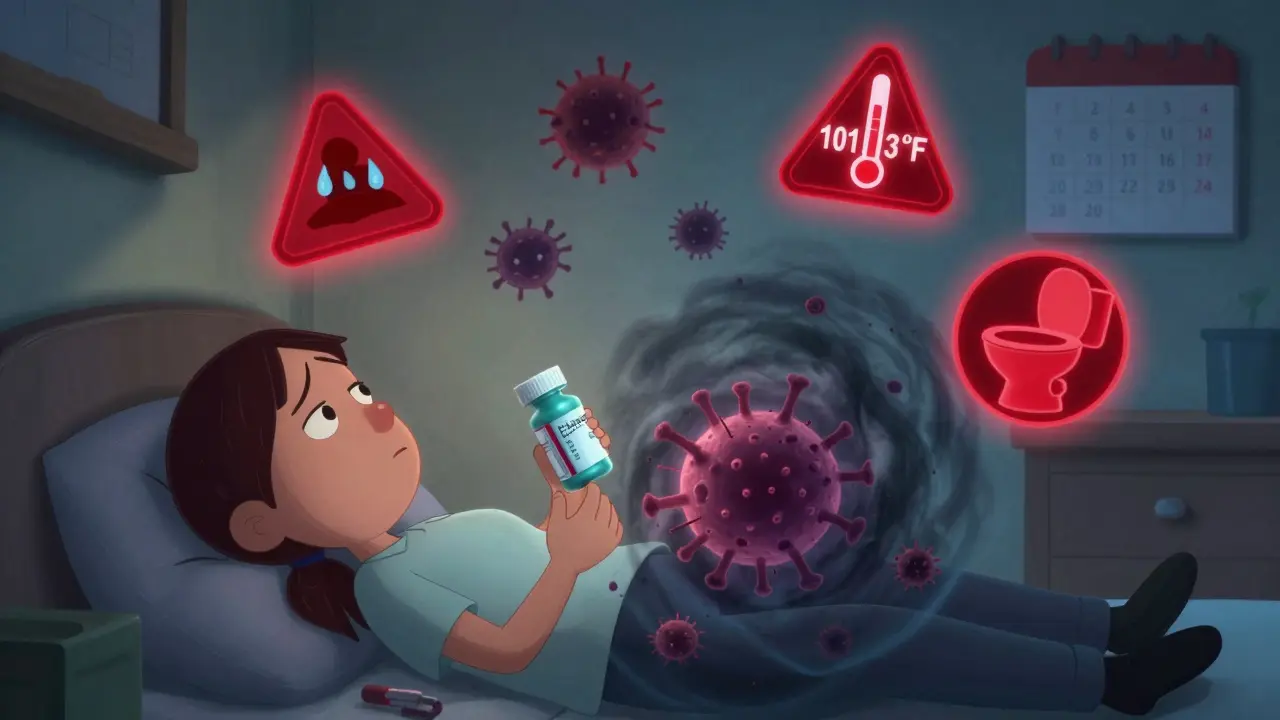
What Symptoms Should You Watch For?
C. diff doesn’t always look like typical diarrhea. Here’s what to watch for:- Three or more loose or watery stools in a 24-hour period
- Abdominal cramping or pain that doesn’t go away
- Fever over 101.3°F (38.5°C)
- Blood or pus in your stool
- Nausea, loss of appetite, or feeling unusually tired
- Signs of dehydration: dark urine, dizziness, dry mouth, or not peeing for 8+ hours

When to Go to the Doctor
Don’t wait. If you’re taking clindamycin or have finished it in the last 12 weeks and you notice any of the symptoms above, call your doctor today. Don’t wait two days. Don’t try antidiarrheal meds like Imodium-they can trap toxins in your gut and make things worse. The CDC and infectious disease guidelines say: if you have three or more unformed stools in 24 hours for two days straight, AND you’ve taken an antibiotic recently, get tested for C. diff. For high-risk patients-older adults, those with prior C. diff, or people on immunosuppressants-don’t wait two days. Call after 24 hours. If you have:- Severe abdominal pain or swelling
- High fever with chills
- Low blood pressure or dizziness
- Not urinating for over 8 hours
- Signs of shock (cold skin, rapid heartbeat, confusion)
What Happens After Diagnosis?
If you test positive for C. diff, your doctor will stop clindamycin right away. Treatment depends on how bad it is:- Mild to moderate cases: usually treated with vancomycin or fidaxomicin
- Severe cases: may need IV antibiotics, fluids, and hospitalization
- Recurrent cases: newer treatments like VOWST (a pill made from bacterial spores) help restore gut balance and prevent future outbreaks

How to Protect Yourself
The best way to avoid C. diff is to avoid unnecessary antibiotics. But if you need clindamycin, here’s what you can do:- Ask your doctor: "Is there a lower-risk antibiotic that would work just as well?" For skin infections, trimethoprim-sulfamethoxazole is often a safer choice. For dental work, amoxicillin is usually fine unless you’re allergic.
- Take probiotics with caution. While some studies suggest they might help, the evidence isn’t strong enough to rely on them alone.
- Wash your hands with soap and water-alcohol-based sanitizers don’t kill C. diff spores.
- Don’t share towels or bathroom items if someone in your home has C. diff.
The Bigger Picture
C. diff isn’t just a personal health issue-it’s a public health crisis. The average hospital stay for C. diff costs over $11,000. Cases tied to clindamycin cost nearly $14,000 because they’re more likely to lead to complications. And while hospital cases have dropped since 2011, community cases have risen by 16%-mostly because of outpatient antibiotic use. The FDA now requires all antibiotic labels to list C. diff risk. Clindamycin’s label now says it’s in the "highest risk" category. Still, doctors prescribe it too often-42% of the time, it’s used when a safer option exists. New drugs like ridinilazole are in trials and show promise for reducing recurrence in clindamycin-exposed patients. But for now, the best defense is awareness.Can clindamycin cause C. diff even after I’ve finished the course?
Yes. C. diff can develop up to 12 weeks after you stop taking clindamycin. Most cases happen within 14 days, but symptoms can appear weeks later. Don’t assume you’re safe just because you’re done with your pills.
Is it safe to take Imodium if I have diarrhea while on clindamycin?
No. Anti-diarrheal medications like Imodium can trap the C. diff toxins inside your intestines, making the infection worse and increasing your risk of serious complications. Stop taking them and call your doctor instead.
Can I get C. diff from someone else?
Yes. C. diff spores spread through feces and can survive on surfaces for months. If someone with C. diff doesn’t wash their hands properly, they can contaminate doorknobs, toilets, or towels. Wash your hands with soap and water, especially after using the bathroom or before eating.
Are there alternatives to clindamycin for dental infections?
Yes. For most dental infections, amoxicillin is the first choice. If you’re allergic to penicillin, clindamycin is often used-but alternatives like azithromycin or metronidazole may be options depending on your allergy history and infection type. Always ask your dentist or doctor about lower-risk choices.
How do I know if I have a severe case of C. diff?
Severe C. diff means you’re at risk of life-threatening complications. Watch for: high fever (over 101.3°F), severe abdominal pain or swelling, low blood pressure, rapid heart rate, not urinating for 8+ hours, or confusion. These are signs you need emergency care immediately.
Will I get C. diff every time I take clindamycin?
No. The absolute risk is low-about 1 to 2% of people who take clindamycin develop C. diff. But because it’s so common, and because the consequences can be so serious, it’s still considered one of the highest-risk antibiotics. The key is knowing the signs so you can act fast if it happens.
Can probiotics prevent C. diff?
Some studies suggest certain probiotics like Lactobacillus or Saccharomyces boulardii might help reduce risk, but the evidence isn’t strong enough to rely on them alone. They shouldn’t replace other precautions like handwashing or avoiding unnecessary antibiotics. Always talk to your doctor before starting any supplement.

Okay but imagine your dentist just hands you a prescription for clindamycin like it’s a lollipop 🍬 and you’re like ‘cool, I’m allergic to penicillin so this is fine’-then three days later you’re on the bathroom floor sobbing into toilet paper because your guts feel like they’re being chewed by a rabid badger. I didn’t even know C. diff could hit you *after* you finished the pills. My mom got it after a tooth extraction and spent a week in the hospital. Don’t let your doctor treat antibiotics like candy. 🚨
Clindamycin has the highest C. diff OR (12.3) among all oral antibiotics. It’s a broad-spectrum lincosamide with prolonged fecal excretion. The gut microbiome disruption is non-negotiable. No probiotic mitigates that. If you’re not testing for toxin A/B in suspected cases, you’re doing harm.
Just wanted to say thanks for laying this out so clearly. I’m in the UK and my GP still prescribes clindamycin like it’s no big deal. I had a bad experience last year after a skin infection-thought it was just a stomach bug. Took me ages to connect the dots. Handwashing with soap? That’s the one thing I’ll never forget now. 🙏
OMG I JUST GOT CLINDAMYCIN YESTERDAY 😱 I’M SO SCARED NOW 💀 I’M ALREADY HAVING LOOSE STOOLS AND I’M JUST STARED AT MY TOILET FOR 20 MINUTES THINKING ‘IS THIS IT??’ 😭 I’M NOT GOING TO WORK TOMORROW I’M GOING TO STARE AT MY BUTT IN THE MIRROR 😭😭😭
So let me get this straight-you’re telling me I can’t take Imodium because it might trap the ‘evil poop demon’ in my colon? But I can take a whole course of antibiotics that literally nukes my gut flora? That’s not a medical protocol, that’s a horror movie script written by a pharmacy rep. 😂
Good breakdown. I work in infection control and see this way too often. Fidaxomicin isn’t just ‘better’-it’s a game-changer for recurrence. The microbiome preservation mechanism? Brilliant. But cost is a barrier. Also, people don’t realize C. diff spores survive on phones, remotes, even keyboards. Disinfect surfaces with bleach-based cleaners. And yes, alcohol gels? Useless against spores. Wash hands. Always.
This made me cry a little. My sister had C. diff after a simple tooth extraction. She was 28. No comorbidities. Just took clindamycin and woke up in the ER three weeks later. I wish I’d known then what I know now. Please, if you’re reading this-ask your doctor for alternatives. Even if they say ‘it’s fine.’ It’s not fine. Your gut is sacred.
One sentence: If you’ve taken clindamycin and have diarrhea-even mild-call your doctor before Googling it. Seriously. Just call.