Every year, millions of people in the U.S. alone are affected by medication errors - and a large chunk of those happen right at the pharmacy counter. It’s not about bad pharmacists. It’s about broken systems. A 2023 global review found that dispensing errors happen in about 1.6% of all prescriptions filled. That might sound small, but when you’re talking about billions of prescriptions annually, that’s hundreds of thousands of mistakes. Some are minor. Others can land someone in the hospital - or worse.
What Are the Most Common Pharmacy Dispensing Errors?
Pharmacists aren’t robots. They’re humans working under pressure, often juggling dozens of prescriptions at once. That’s when things go wrong. The biggest errors fall into a few clear categories.The most frequent mistake? Giving the wrong medication, dose, or form. This accounts for about 32% of all dispensing errors. Think: handing out amoxicillin instead of azithromycin. Or giving a 500mg tablet when the prescription called for 250mg. Or dispensing a capsule when the patient needs a liquid form because they can’t swallow pills.
Second biggest? Miscalculating the dose. This happens a lot with kids, elderly patients, or people with kidney or liver problems. A dose that’s safe for a 70kg adult could be deadly for a 45kg senior with reduced kidney function. Yet, without checking lab values or weight, pharmacists might miss it.
Third? Failing to catch dangerous drug interactions. One in four dispensing errors happens because a pharmacist didn’t realize the new prescription clashes with something the patient is already taking. For example, mixing warfarin with certain antibiotics can cause dangerous bleeding. Or combining opioids with benzodiazepines - a combo that’s killed thousands.
Other common mistakes include:
- Dispensing expired meds because they weren’t rotated properly in stock
- Giving the wrong duration - like filling a 30-day supply when the doctor ordered 14 days
- Wrong route - handing out an oral tablet when the prescription was for an injection
- Wrong strength - grabbing a 10mg bottle instead of a 5mg one because they look identical
- Wrong rate - IV meds given too fast, like vancomycin causing red man syndrome
Some drugs are far more dangerous when messed up. Anticoagulants like warfarin and rivaroxaban are involved in 31% of serious errors. Opioids? 24%. Antibiotics? 28%. And in 41% of antibiotic-related errors, the pharmacist never checked the patient’s allergy history.
Why Do These Errors Keep Happening?
It’s not because pharmacists are careless. It’s because the system is stacked against them.Workload is the #1 culprit. Nearly 37% of errors happen because pharmacists are overwhelmed - rushing between filling scripts, answering phones, counseling patients, and managing inventory. One pharmacist in Manchester told me: "I had 120 prescriptions to fill by 11 a.m. I didn’t have time to double-check every one."
Sound-alike and look-alike drugs are another huge problem. Drugs like hydroxyzine and hydralazine, or lorazepam and labetalol, look almost identical on the shelf. Even the packaging is similar. In handwritten prescriptions, this gets worse. One study found that 19% of errors came from misreading handwriting - and 22% came from verbal prescriptions where "Zoloft" was heard as "Zyloft."
Interruptions are deadly. If a pharmacist is interrupted three or more times while filling a script, the chance of an error jumps by over 12%. That’s why many pharmacies now have "do not disturb" zones during high-risk fills.
Missing information is a silent killer. Forty-three percent of errors stem from unclear or incomplete prescriptions. A doctor writes "take one daily" but doesn’t specify the strength. Or the patient’s allergy isn’t in the system. Or their kidney function wasn’t updated after their last blood test. Pharmacists are expected to fill in the blanks - and they can’t always do it safely.

How to Stop These Errors: Proven Prevention Strategies
The good news? Most of these errors are preventable. And the solutions aren’t sci-fi - they’re practical, tested, and already working in pharmacies across the UK and U.S.1. Double-check high-alert medications. Insulin, heparin, warfarin, opioids, and IV potassium are on the "high-alert" list for a reason. One hospital pharmacy in Manchester cut their insulin errors by 78% by requiring two pharmacists to verify every single one before it leaves the counter. No exceptions.
2. Use barcode scanning. Barcoding isn’t new, but it’s still underused. A 2023 survey of 127 U.S. hospitals found that barcode systems reduced dispensing errors by nearly half. They caught wrong drugs (52% fewer), wrong doses (49% fewer), and wrong forms (45% fewer). Even community pharmacies using handheld scanners saw 12 serious errors caught in their first month.
3. Implement Tall Man lettering. This is simple: write similar drug names differently to make them stand out. Instead of "prednisone" and "prednisolone," use "PREDNISone" and "prednisoLONE." This visual cue reduces confusion. Pharmacies that adopted this saw a 57% drop in sound-alike errors.
4. Build in mandatory checks for allergies and kidney function. Before dispensing any antibiotic, anticoagulant, or NSAID, the system should auto-flag: "Check allergy history." "Check eGFR." "Check weight." If the data isn’t there, the script shouldn’t be filled. This simple rule stopped 72% of allergy-related errors in one large pharmacy chain.
5. Use clinical decision support tools. Modern pharmacy software doesn’t just count pills - it warns you. If you try to dispense metformin to a patient with an eGFR below 30, the system should pop up: "Contraindicated. Renal impairment."
6. Reduce interruptions. Designate quiet zones during peak hours. Use status lights: green = free, red = busy. Train staff to respect "do not disturb" signals. One pharmacy in Leeds cut their error rate by 31% just by limiting interruptions during high-risk fills.
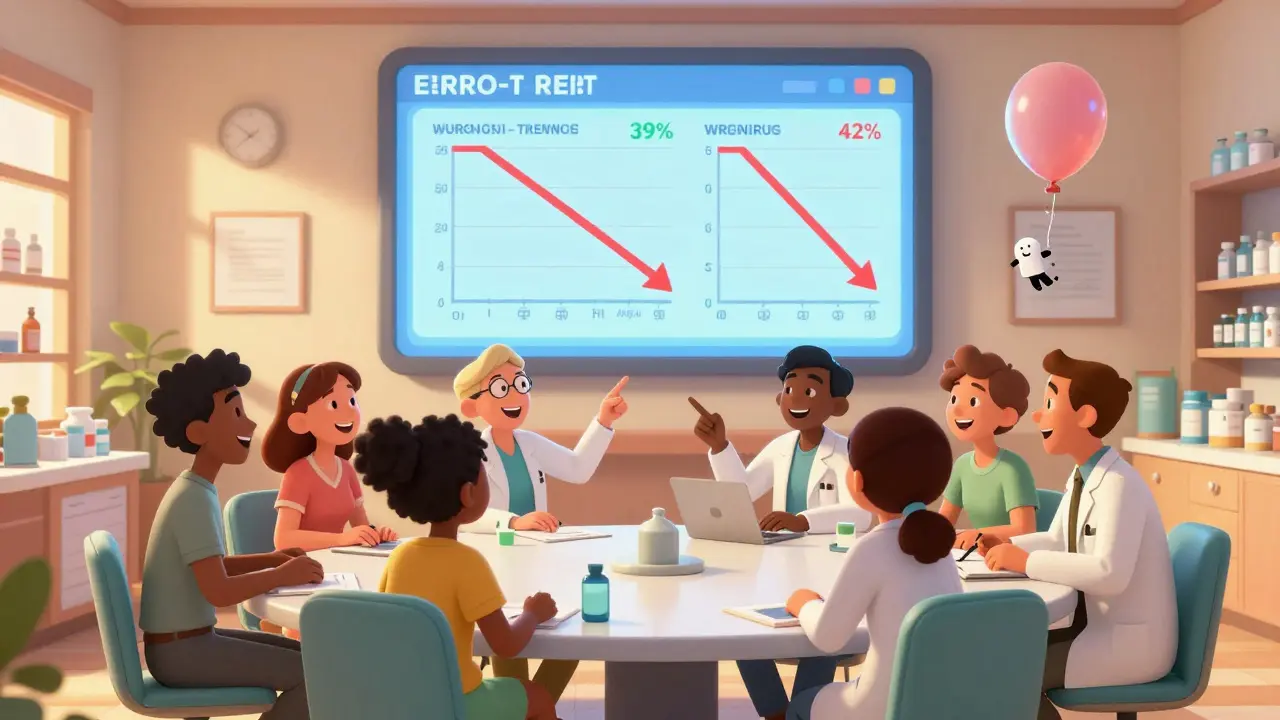
7. Report and learn from mistakes. The best pharmacies don’t punish errors - they study them. Systems like Pharmapod let pharmacists anonymously log every near-miss and actual error. Within a year, pharmacies using this tool saw a 39% drop in wrong-strength errors and 42% fewer wrong-drug errors. Learning from mistakes beats blaming people.
Technology Isn’t the Whole Answer
You might think: "Just automate everything." But technology can create new problems.Computerized prescribing systems (CPOE) cut errors by 43% - but introduced new ones in 18% of cases. Why? Alert fatigue. If your system pings you with 50 warnings per shift, you start ignoring them. One pharmacist said: "I stopped reading the pop-ups. I was tired of being yelled at for every little thing."
Robotic dispensing systems cut errors by 63% - but cost between $150,000 and $500,000. Most community pharmacies can’t afford them. And they don’t fix the root issue: poor communication between doctors, pharmacists, and patients.
Artificial intelligence is promising. One trial in 34 hospitals used AI to predict which prescriptions were most likely to have errors - and flagged them for extra review. They cut errors by over 52%. But AI needs clean data. If the patient’s weight or allergies are missing from the EHR, the AI can’t help.
The real solution? A hybrid. Use tech to catch the easy mistakes. Use humans to catch the complex ones. Let the machine handle barcodes and alerts. Let the pharmacist focus on the patient: "Are you taking anything else? How’s your kidney doing? Did you have a reaction to this before?"
What Patients Can Do
You’re not powerless. Even if the system fails, you can protect yourself.- Always ask: "Is this the same as what I got last time?" If it looks different, question it.
- Check the label. Does the name, dose, and instructions match what your doctor told you?
- Ask: "What is this for?" If the pharmacist says, "It’s for your blood pressure," but you were prescribed it for an infection - speak up.
- Keep a list of all your meds - including OTC and supplements - and bring it to every appointment.
- If you’re unsure, call your pharmacist back. They’re paid to answer questions. Don’t feel silly.
One woman in Manchester saved herself from a dangerous interaction by asking: "This new pill says it’s for cholesterol. But I’ve never had high cholesterol. Why am I taking it?" The pharmacist checked - the doctor had accidentally prescribed simvastatin instead of simethicone. The error was caught before she took a single pill.
The Future Is Clearer - But We Need to Act Now
By 2025, 78% of U.S. pharmacies will use standardized error classification systems. The WHO and ISMP are finalizing a global reporting system expected in early 2025 - this will help countries learn from each other instead of repeating the same mistakes.But progress won’t come from fancy machines alone. It comes from culture. From systems that assume humans will make mistakes - and build safeguards around that. From pharmacies that reward reporting over punishment. From doctors who write legibly and include full details.
Every dispensing error is a system failure - not a person failure. Fix the system, and the errors drop. Blame the pharmacist, and they’ll keep burning out.
The data is clear: with simple, smart changes, we can cut these errors by more than half. We know how to do it. Now we just need to do it - consistently, everywhere.


This is the kind of post that makes me want to scream into a pillow. I’ve had my meds mixed up twice, and both times I only caught it because I was paranoid enough to double-check the bottle. One time I almost took a blood pressure pill thinking it was my thyroid med. No one apologized. No one even seemed surprised.
Let me tell you something - this isn’t just about pharmacies. This is about a system that treats human beings like numbers on a spreadsheet. I’ve seen nurses cry because they had to rush through 80 scripts before lunch. Pharmacists aren’t gods. They’re overworked, underpaid, and expected to be perfect while the system crumbles around them. We need to stop blaming the people and fix the machine.
you know what really causes these errors the government forcing pharmacies to use electronic records that dont talk to each other and then blaming the pharmacist when the computer glitches and gives you the wrong pill its not the pharmacist its the corporate greed behind the software companies
While the systemic issues outlined in this post are indeed profound and warrant urgent attention, I would like to emphasize the importance of structured, evidence-based interventions grounded in clinical governance frameworks. The implementation of standardized protocols, coupled with continuous professional development, remains indispensable in mitigating dispensing errors at scale.
so like... the system is broken but we still expect the pharmacist to be a superhero? lol. theyre not even paid enough to afford therapy after dealing with this mess. also why is no one talking about how the insurance companies force pharmacies to fill 200 scripts an hour? its not magic its math and the math is terrible
It’s fascinating how we’ve built a society that can land robots on Mars but can’t design a pharmacy workflow that doesn’t risk someone’s life because of a typo or a misread script. We optimize for efficiency, not safety. We reward speed over scrutiny. We treat human error as a moral failing instead of a predictable outcome of poorly designed systems. If we built bridges like we build pharmacy workflows, we’d all be dead. And yet we’re shocked when someone gets the wrong pill. We’re not just failing pharmacists - we’re failing each other.
so i just got my script filled and the label says "take 1 pill 3x a day" but the bottle says "take 1 pill 2x a day" and i’m supposed to trust this? and then they say "oh we have a barcode system" like that’s magic? i scanned it twice and the scanner didn’t say a thing. also why is my antibiotic labeled "for acne" when i have a UTI? i’m not dumb i just want to live
These problems don’t exist in America because we have the best healthcare system in the world. If you’re getting the wrong meds, maybe you’re not paying enough attention. The real issue is that people in other countries don’t have the resources to fix this - but here, we’re talking about a few bad apples, not a broken system. Stop whining and take responsibility.
While the prevalence of dispensing errors is alarming, it is imperative to recognize that technological interventions - such as barcode scanning and clinical decision support - are not silver bullets. Their efficacy is contingent upon user adherence, system integration, and organizational culture. Without sustained training and leadership commitment, even the most advanced tools will fail to deliver their intended safety benefits.
I’ve worked in community pharmacy for 18 years. I’ve seen everything - the handwritten scribbles, the interrupted fills, the allergy lists that haven’t been updated since 2012. But I’ve also seen what happens when you give pharmacists time, respect, and tools. We implemented double-checks for high-alert meds in my shop. We added a quiet zone. We started asking patients: "What’s your story?" And guess what? Errors dropped. Not because we’re heroes - because we were finally allowed to be professionals.
This entire post is a thinly veiled attack on American healthcare superiority. In nations with universal systems, errors are far less common because there is centralized oversight, standardized training, and mandatory reporting. The fact that this is even a discussion in the U.S. speaks volumes about our fragmented, profit-driven model. It is not incompetence - it is systemic decay.
Hey - if you’re reading this and you’re a patient: PLEASE keep a medication list. Write it down. Bring it in. Don’t rely on memory. I had a woman come in last week who was on 17 meds - and she couldn’t remember half of them. We caught a dangerous interaction between her blood thinner and her new OTC fish oil. That’s the power of a simple list. And if you’re a pharmacist? You’re not alone. We’re in this together. Speak up. Report near-misses. You’re saving lives - even if no one claps.
barcodes help. tall man letters help. asking patients simple questions helps. none of this is rocket science. we just need to stop pretending the problem is the people and start fixing the environment they work in
That woman in Manchester who asked about the cholesterol pill? That’s my mom. She’s 74. She doesn’t know what simvastatin is. But she knows it doesn’t look right. She’s not a nurse. She’s just not willing to die because someone else didn’t check.