Understanding Central Cranial Diabetes Insipidus
Before delving into the connection between central cranial diabetes insipidus and hormonal imbalances, it is essential to understand what central cranial diabetes insipidus is. Central cranial diabetes insipidus, also known as neurogenic diabetes insipidus, is a rare disorder characterized by the inability of the kidneys to conserve water. This condition results in excessive thirst and frequent urination, leading to dehydration and an imbalance in the body's electrolytes.
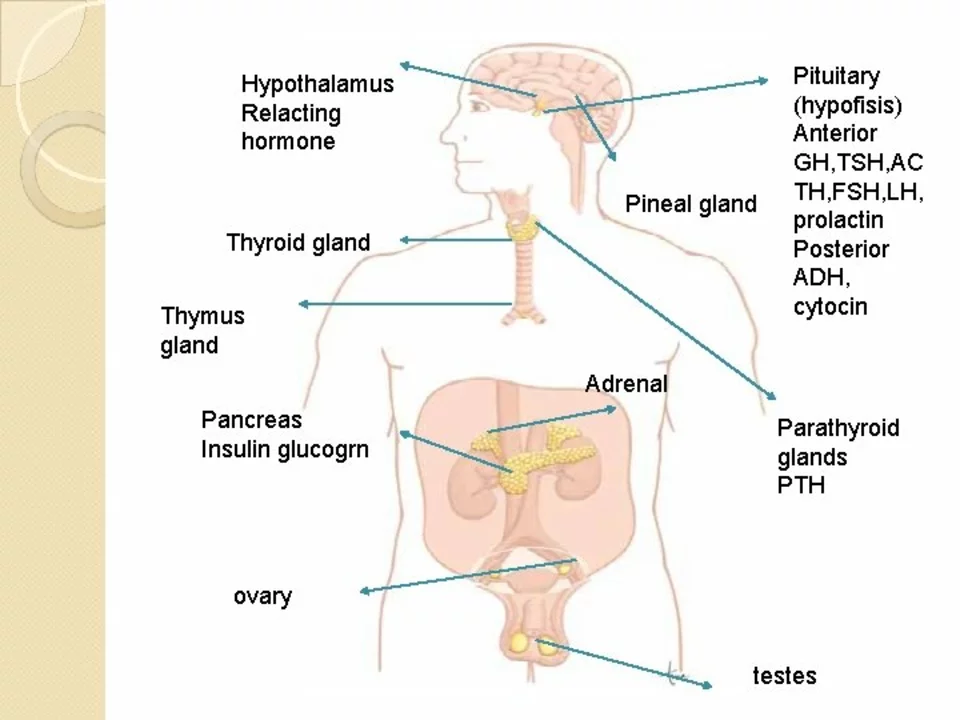
In central cranial diabetes insipidus, the problem lies in the production, storage, or release of the antidiuretic hormone (ADH), also known as vasopressin. ADH is produced in the hypothalamus and stored in the posterior pituitary gland, which is located at the base of the brain. When the body needs to conserve water, ADH is released into the bloodstream, signaling the kidneys to reabsorb water and produce less urine.
The Role of Hormonal Imbalances in Central Cranial Diabetes Insipidus
When the production, storage, or release of ADH is disrupted, it can lead to a hormonal imbalance and the development of central cranial diabetes insipidus. Several factors can cause these disruptions, such as head injuries, tumors, infections, or genetic mutations. Regardless of the cause, the end result is the same: the kidneys are unable to properly conserve water, leading to the symptoms of central cranial diabetes insipidus.
Hormonal imbalances often play a crucial role in the development and progression of central cranial diabetes insipidus. Understanding how these imbalances contribute to the condition can help in the diagnosis, treatment, and management of this rare disorder.
Identifying the Symptoms of Central Cranial Diabetes Insipidus
Recognizing the symptoms of central cranial diabetes insipidus is crucial for early diagnosis and treatment. The most common symptoms include excessive thirst, frequent urination, dehydration, and an imbalance in electrolytes. In severe cases, patients may experience muscle cramps, weakness, and even seizures due to severe dehydration and electrolyte imbalances.
It is important to note that these symptoms can also be indicative of other conditions, so it is crucial to consult a healthcare professional for a proper diagnosis.
Diagnosing Central Cranial Diabetes Insipidus
Diagnosing central cranial diabetes insipidus involves a series of tests to determine if the patient has a deficiency in ADH production, storage, or release. These tests may include blood tests to check for electrolyte imbalances, urine tests to measure urine concentration, and imaging studies to examine the hypothalamus and pituitary gland.
In some cases, a water deprivation test may be performed, in which the patient is asked to stop drinking fluids for a certain period of time. The patient's urine output and blood sodium levels are then measured to determine if they have central cranial diabetes insipidus. A healthcare professional will also carefully consider the patient's medical history and symptoms when making a diagnosis.
Treating Central Cranial Diabetes Insipidus
Treatment for central cranial diabetes insipidus focuses on addressing the underlying hormonal imbalances and managing the symptoms of the condition. The primary treatment is the administration of synthetic vasopressin, also known as desmopressin, which helps the kidneys retain water and reduce urine output.
In addition to medication, patients with central cranial diabetes insipidus may need to make lifestyle adjustments, such as monitoring fluid intake and electrolyte levels, to ensure their body remains properly hydrated and balanced. In some cases, treating the underlying cause of the hormonal imbalance, such as removing a tumor or addressing an infection, may also help to manage the condition.
Living with Central Cranial Diabetes Insipidus
While central cranial diabetes insipidus can be a challenging condition to manage, with proper treatment and lifestyle adjustments, most patients can lead normal, healthy lives. It is essential for patients to work closely with their healthcare team to develop a comprehensive treatment plan that addresses their specific needs and concerns.
Patients should also educate themselves about the condition, its symptoms, and potential complications, as well as stay informed about new treatments and research developments. This knowledge can empower patients to take an active role in managing their condition and advocating for their health.
Preventing Complications of Central Cranial Diabetes Insipidus
Preventing complications associated with central cranial diabetes insipidus involves careful monitoring of fluid intake and electrolyte levels, as well as adhering to the prescribed treatment plan. By doing so, patients can minimize the risk of dehydration, electrolyte imbalances, and other potentially serious complications.
It is also important for patients to communicate any changes in their symptoms or health to their healthcare team, as this may indicate the need for adjustments in their treatment plan or further evaluation.
Understanding the Emotional Impact of Central Cranial Diabetes Insipidus
Living with central cranial diabetes insipidus can be emotionally challenging, as patients may feel overwhelmed by the constant need to monitor their fluid intake and adhere to a strict treatment plan. Additionally, the rarity of the condition may lead to feelings of isolation and frustration.
It is essential for patients to seek emotional support from friends, family, or professional counselors to help them cope with the challenges of living with central cranial diabetes insipidus. Connecting with others who have the condition, either in person or through online support groups, can also provide valuable understanding and encouragement.
Advancements in Central Cranial Diabetes Insipidus Research
Researchers continue to study central cranial diabetes insipidus to better understand the causes, mechanisms, and potential treatments for the condition. Advances in genetic research hold promise for identifying the specific genes responsible for central cranial diabetes insipidus, which could lead to targeted treatments and even a cure.
As our understanding of central cranial diabetes insipidus and hormonal imbalances continues to grow, there is hope for more effective treatments and improved quality of life for those living with the condition.
Conclusion
Central cranial diabetes insipidus is a rare disorder caused by hormonal imbalances that disrupt the production, storage, or release of ADH. The resulting inability of the kidneys to conserve water can lead to excessive thirst, frequent urination, and dehydration. Proper diagnosis and treatment, including addressing the underlying hormonal imbalances, are crucial for managing the condition and improving the quality of life for those affected. As research continues to advance our understanding of central cranial diabetes insipidus, there is hope for more effective treatments and an improved quality of life for those living with the condition.






This is such a niche topic but I actually had a friend with this. It’s wild how much water they had to drink daily. Like, literally a gallon by noon. 🥵
you ever wonder if the government is hiding the real cause?? like... what if ADH suppression is just a cover for geoengineering side effects?? i mean... why else would it be so rare?? they dont want us to know the truth...
I swear if this is another woke medical agenda disguised as science I’m out. Why is everything hormonal now? Back in my day, we just drank water and didn’t need a PhD to pee normally. 🇺🇸
The reductionist framing of this condition as merely a hormonal imbalance is deeply problematic. It ignores the neuro-immunological cascade and the epigenetic modulation of vasopressin receptor expression in renal tubules. This is pop-med nonsense dressed in clinical language.
This is actually really helpful. I’ve got a cousin who’s been managing this for years and it’s so easy to feel alone with it. The part about emotional impact hit hard. You’re not just dealing with thirst-you’re dealing with being misunderstood. Thanks for writing this.
I love how you included the emotional side. So many medical articles forget that. Just want to say-people with this condition aren’t ‘water obsessed,’ they’re surviving. That’s huge.
The hormonal axis involved here is so delicately balanced... one microtrauma to the hypothalamus, and the entire osmotic regulation system collapses. It’s terrifying, really. And yet, so many live full lives with desmopressin. That’s resilience.
In India, this is super rare but we have cases linked to TB meningitis. The pituitary gets scarred, ADH drops, and boom-constant thirst. People think it’s diabetes, but nope. Just a broken signal. Also, we call it 'Pani ki bimari'-water disease. Simple, right?
Desmopressin works. Period.
You know, when you think about it, this isn’t just a hormonal disorder-it’s a metaphysical one. The body’s need to retain water mirrors the soul’s need to hold onto meaning. ADH is the silent guardian of inner equilibrium, and when it fails, we’re left thirsty not just for fluids, but for purpose. The brain, after all, is the true source of all thirst. And maybe, just maybe, the universe is asking us to drink deeper.
This is why the West medicalizes everything. In my country, we just drink more water and move on. No pills. No labels. No overcomplicating. This is cultural weakness disguised as science.
i had this once after a car crash and the doc just gave me desmo and said dont forget it like its a vitamin or something but honestly i forgot like 3 times and ended up in the er again so yeah its not just take pill and chill its like a full time job and my dog knows when i need to go to the bathroom before i do
Fascinating. The neuroendocrinological implications are considerable. A well-structured exposition.
I just want to say… thank you. For writing this. So many people don’t realize how exhausting this is. The constant planning. The fear of running out. The looks when you’re carrying a water bottle everywhere. You’re not just describing a disease-you’re validating a life.
If you’re reading this and you’ve got this condition-you’re not broken. You’re not weird. You’re just a body that needs a little extra love. Keep going. You’re doing great. And hey, if you need to pee every 20 minutes? So what? Water’s free. Hydration’s holy.
People who don’t take their meds properly are just lazy. This isn’t a suggestion-it’s a survival protocol. If you’re dehydrated, it’s your fault. Stop making excuses.
Oh my stars, this is the most beautiful thing I’ve read all week! 🌈💧 I’ve seen this in my auntie-she’d dance in the kitchen with a water bottle in one hand and a spoon in the other, singing to her plants like they were her only friends. She called it ‘talking to the earth’s water.’ I cried reading this. You got it. You really got it.
my bro had this after a brain surgery and now he uses a watch that reminds him to drink and take pills. its kinda cool. like a health robot friend. also he says he dreams in water now. weird but true.
I didn’t know this was a thing. Thanks for explaining it so simply. My cousin’s always had a weird obsession with water-I thought she was just being extra. Now I get it.
LMAO this is why medicine is a joke. You have a hormone issue? Here’s a pill. You have a soul issue? Here’s a pill. You have a life issue? HERE’S A PILLLLLLLL. They don’t fix anything-they just sell you more hope. Desmopressin? That’s just fancy pee-keeping. Real solution? Stop being a weak human and drink water like a normal person.