What Is Otitis Media?
Otitis media is an infection or inflammation of the middle ear, the space behind the eardrum that’s filled with air and connected to the throat by the Eustachian tube. It’s one of the most common reasons parents take their kids to the doctor-especially under age 3. In fact, more than 80% of children have at least one ear infection by their third birthday, according to the Children’s Hospital of Philadelphia. The infection happens when fluid gets trapped behind the eardrum, often after a cold or allergy flare-up. That fluid becomes a breeding ground for bacteria or viruses, leading to pain, pressure, and sometimes fever.
Why Do Kids Get Ear Infections More Than Adults?
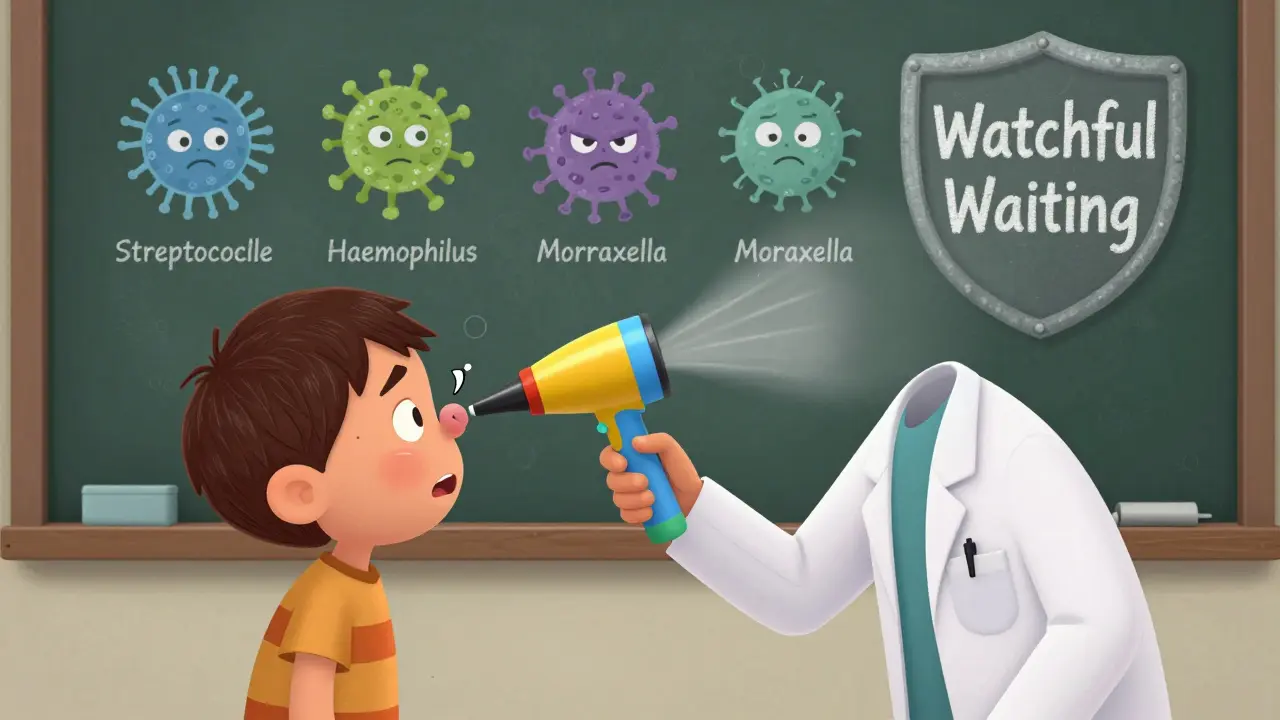
It’s not just bad luck. Kids’ Eustachian tubes are shorter, more horizontal, and less developed than adults’. That means they don’t drain fluid as well. When a child gets a cold, the tubes swell and get blocked. Fluid builds up. Bacteria like Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis move in. In adults, the tubes are angled downward and more efficient at clearing fluid, so infections are rarer.
Other risk factors include:
- Exposure to cigarette smoke (raises risk by about 50%)
- Bottle-feeding while lying down (breastfeeding upright reduces risk)
- Attending daycare (kids there are 2-3 times more likely to get infections)
- Living in areas with high air pollution
How Do You Know It’s an Ear Infection?
Not every ear tug or fuss means infection. But if your child has:
- Sudden crying, especially at night
- Fever over 100.4°F (38°C)
- Fluid draining from the ear
- Difficulty sleeping or pulling at the ear
- Loss of appetite or trouble hearing
-it could be acute otitis media (AOM). Doctors check for this with a pneumatic otoscope, which blows a puff of air at the eardrum. If it doesn’t move well, fluid is likely trapped behind it. The eardrum may look red and bulging. In some cases, hearing tests show a mild conductive hearing loss-15 to 40 decibels-which usually goes away once the infection clears.
Antibiotics: When Are They Really Needed?
Here’s the big shift in medical thinking: not every ear infection needs antibiotics. A 2022 update from the American Academy of Pediatrics and the American Academy of Family Physicians says that for many kids, watchful waiting is safer and just as effective.
Antibiotics work best for:
- Children under 6 months with confirmed infection
- Kids 6 to 23 months with severe symptoms (fever above 102.2°F or ear pain lasting more than 48 hours)
- Children 2 years and older with severe pain or high fever
For milder cases-especially in older kids-the body can often fight it off on its own. Studies show that 80% of uncomplicated ear infections clear up within 3 days without antibiotics. That’s why many pediatricians now recommend waiting 48 to 72 hours before prescribing, especially if the child isn’t in extreme pain or running a high fever.
What Antibiotics Are Used-and Which Ones Work Best?
When antibiotics are needed, amoxicillin is still the first choice. The recommended dose is 80-90 mg per kg of body weight per day, split into two doses. For kids under 2 with bilateral infections, a full 10-day course is standard. For older kids with mild symptoms, 5-7 days may be enough.
If a child is allergic to penicillin, alternatives include:
- Cefdinir (oral)
- Ceftriaxone (single shot)
- Azithromycin (5-day course)
Amoxicillin-clavulanate (Augmentin) is sometimes used if the infection doesn’t improve with amoxicillin, but resistance is rising. In 2022, 12.4% of Haemophilus influenzae strains were resistant to it-up from 7.2% in 2010. That’s why doctors are cautious about overusing it.
What About Side Effects?
Antibiotics aren’t harmless. About 1 in 5 kids get diarrhea. Rashes happen in 5-10% of cases. Some kids vomit or lose their appetite. Parents on parenting forums often mention how hard it is to get liquid antibiotics down a screaming toddler. And every unnecessary course adds to the global problem of antibiotic resistance.
The CDC reports that 30-50% of Streptococcus pneumoniae strains in the U.S. are resistant to penicillin. That’s why high-dose amoxicillin is still effective-it overwhelms the resistant bugs. But if we keep prescribing antibiotics when they’re not needed, even that might stop working.
Pain Relief: The Real First Step
Before you even think about antibiotics, focus on pain control. That’s what matters most to your child. Use:
- Acetaminophen (10-15 mg per kg every 4-6 hours)
- Ibuprofen (5-10 mg per kg every 6-8 hours)
Many parents report that ibuprofen made the difference between a crying, sleepless night and a child who could rest. Warm compresses on the ear can help too. Some doctors recommend ear drops like Auralgan, but only if the eardrum isn’t ruptured. Never put anything in the ear if you see pus or fluid leaking-that’s a sign of a burst eardrum, and you need to see a doctor right away.
When to Worry: Red Flags
Most ear infections resolve without trouble. But call your doctor or go to urgent care if your child has:
- Fever above 104°F (40°C)
- Severe pain that doesn’t improve with painkillers
- Drainage of pus or blood from the ear
- Dizziness, vomiting, or trouble walking
- Facial drooping or weakness
These could mean the infection has spread or caused complications like a ruptured eardrum or mastoiditis. Rare, but serious.
What About Fluid Behind the Eardrum?
After an infection clears, fluid can linger for weeks or even months. This is called otitis media with effusion (OME). It’s not an active infection-it doesn’t cause pain or fever. But it can make hearing fuzzy. The good news? In 90% of cases, the fluid goes away on its own within 3 months. Antibiotics won’t help it. Neither will decongestants or antihistamines. The only time it’s treated is if it lasts longer than 3 months and affects speech development or hearing. Then, a specialist might recommend ear tubes.
Vaccines and Prevention
One of the most effective ways to prevent ear infections? Vaccines. The pneumococcal conjugate vaccine (PCV13) has cut vaccine-type ear infections by 34%. The newer 15-valent vaccine (Vaxneuvance), approved in 2021, looks even better in trials. Flu shots also help-since flu often leads to ear infections.
Other prevention tips:
- Breastfeed upright if possible
- Avoid smoke exposure
- Limit daycare exposure during peak cold season
- Wash hands often
What’s Next for Treatment?
Doctors are moving toward smarter, faster diagnosis. Smartphone otoscopes like CellScope Oto let parents take pictures of the eardrum and send them to a doctor. Studies show they’re 85% accurate. In-office tympanometry (a test that measures eardrum movement) is becoming more common and has cut unnecessary antibiotic prescriptions by 22% in young kids.
Looking ahead, experts predict point-of-care tests that identify the exact bacteria causing the infection within minutes. That could cut broad-spectrum antibiotic use by 30-40% in the next five years. For now, the best approach is still: wait, watch, and treat pain-unless the signs point clearly to a serious infection.
What Parents Are Saying
Online forums are full of mixed experiences. One parent on Reddit wrote: "We waited 48 hours. The fever broke. The crying stopped. No antibiotics needed. No diarrhea, no fuss." Another shared: "After 72 hours, my toddler spiked a 104°F fever and ended up in the ER with a ruptured eardrum. I wish we’d started antibiotics sooner." The truth? Both stories are valid. The key is knowing your child’s symptoms, trusting your gut, and working with your doctor to decide when to wait-and when to act.


Man, I remember my little cousin in Delhi getting ear infections every monsoon. We’d use warm mustard oil drops-old-school, but it worked. No antibiotics unless the fever hit 103+. Kids’ bodies are tougher than we think.
Also, daycare? Total germ vortex. My sister switched to home-based care and her kid hasn’t had one in two years.
The real win here isn’t the antibiotics-it’s the paradigm shift. We’ve been treating ear infections like they’re bacterial invasions that need a military strike, when 80% of the time, it’s just a viral storm that clears on its own. Pain management isn’t a backup plan-it’s the frontline.
It’s like treating a sprained ankle with a cast instead of ice and rest. We’ve been doing it backward for decades.
Amoxicillin at 80–90 mg/kg/day is still the gold standard for AOM. The pharmacokinetics are well-documented-serum concentrations exceed MIC for S. pneumoniae and H. influenzae for >40% of the dosing interval.
Augmentin resistance is climbing due to beta-lactamase production, especially in H. influenzae. PCV13 reduced vaccine-type otitis by 34%, but non-vaccine serotypes are filling the niche. Surveillance data from CDC’s EARS-NET shows regional variation in resistance patterns-local epidemiology matters.
Oh great. So now we’re supposed to just ‘wait and watch’ while our kids scream through the night like they’re being tortured? Because apparently, doctors don’t know what they’re doing anymore.
My kid got a ruptured eardrum after 72 hours of ‘watchful waiting.’ You think the ER nurse was like, ‘Oh, you followed guidelines?’ No. She said, ‘You’re lucky he didn’t get meningitis.’
And don’t even get me started on the ‘vaccines prevent ear infections’ lie. My son had all his shots. Still got three infections in six months. Who’s really profiting here? Pharma? The CDC? The pediatricians who get paid for prescriptions?
Y’all are overcomplicating this. If your kid’s crying nonstop, can’t sleep, and has a fever-give ‘em ibuprofen. Wait 48 hours. If they’re still wrecked? Call the doc. If they’re back to playing with Legos? You just saved them from diarrhea, yeast rashes, and antibiotic resistance.
It’s not rocket science. It’s parenting. And honestly? The fact that we’re even debating this is kinda wild. We used to just rub warm olive oil on their ears and pray. Now we’ve got smartphone otoscopes and resistance stats. We’re overmedicating because we’re scared, not because it’s necessary.
I’m curious about the tympanometry stats mentioned. If it cuts unnecessary prescriptions by 22%, why isn’t it standard in every pediatric office? Is it cost? Training? Or just inertia?
Also, the 15-valent pneumococcal vaccine-Vaxneuvance-has shown promise in early trials for reducing non-vaccine serotype carriage. But real-world data is still sparse. Are we seeing a drop in recurrent OME yet? Or is this just another incremental win that won’t change clinical practice until the next guideline update?
If you dont give antibiotics for every ear infection you are putting your child at risk period end of story
Parents who wait are gambling with their kids hearing and brain development
And dont even get me started on how the AAP is just following pharma money now
My cousin lost 30% hearing in one ear because they waited too long
I had to take my daughter to the ER because the doctor said 'wait.' The next day she had a 104.5 fever and was vomiting. The ENT said the eardrum was about to burst.
They gave her a shot of ceftriaxone and she cried for two hours. I cried for two weeks.
Don’t tell me to 'trust the process.' The process almost broke my kid.
In India, we have a different approach. Ayurvedic ear drops with neem and turmeric are commonly used in rural areas. While not clinically validated, they are culturally embedded and reduce parental anxiety. Antibiotics are reserved for cases with purulent discharge or systemic signs.
Also, bottle-feeding while lying down is a major risk factor in urban slums where infant positioning is neglected. Community health workers now educate mothers on upright feeding-reduction in incidence observed in pilot programs.
Honestly? I just use the CellScope Oto app now. Took a pic of my son’s ear last week, sent it to his pediatrician. They said 'looks like fluid, no redness, no bulge'-no visit needed. Saved me $200 and a 3-hour wait.
And yeah, ibuprofen is magic. Like, actual magic. He was screaming at 11pm. Gave him a dose. Fell asleep by 11:30. No antibiotics. No drama. Just... chill.
The real issue is not antibiotics-it is the erosion of parental authority. We have allowed medical institutions to dictate how we care for our children. This 'watchful waiting' is a form of passive control.
What is next? 'Wait' before giving Tylenol for fever? 'Wait' before feeding a sick child?
The West has become weak. We treat symptoms like moral failings. We fear medicine. We fear action. We fear responsibility.
America’s obsession with 'natural' and 'wait-and-see' is why we’re losing the war on superbugs. We let parents delay treatment because it’s trendy. Meanwhile, in China and Germany, they hit ear infections with targeted antibiotics on day one.
Our healthcare system is broken. We prioritize 'less intervention' over actual outcomes. We don’t want to be seen as overprescribing-we want to be seen as woke.
My son got his third infection at 18 months. We gave him amoxicillin on day one. He was back to wrestling his dog by day three.
Stop pretending we’re saving the planet by letting kids suffer.
I’m a pediatric nurse and I’ve seen both sides. The kid who cried all night, got ibuprofen, slept for 8 hours, and woke up smiling? That’s the win. The kid who got antibiotics and ended up with a yeast diaper rash and diarrhea? That’s the loss.
But here’s what no one talks about-parents feel guilty if they don’t do something. So we give them a script even when it’s not needed. We’re not just treating ears-we’re treating anxiety.
And honestly? I love that we’re finally starting to normalize 'doing nothing' as a valid medical decision. It’s not lazy. It’s smart.
I’m Canadian and we’ve been doing this watchful waiting thing since the 2000s. Guess what? Our antibiotic resistance rates are LOWER than the U.S.
My daughter had two ear infections by age 2. Both times we waited 48 hours. Both times, she got better. We used ibuprofen, warm compresses, and cuddles. No antibiotics. No drama.
And yeah, I cried when she screamed. But I didn’t give her a pill just to feel like I was doing something.
Stop making this about fear. Make it about trust. Trust your kid’s body. Trust your gut. Trust the science. And for god’s sake, stop letting fear make decisions for you.