Every 40 seconds, someone in the U.S. has a stroke. And while many people know strokes are serious, few understand the real difference between the two main types - and how to stop them before they happen. You can’t afford to guess. Knowing whether it’s an ischemic or hemorrhagic stroke could mean the difference between life and death - or recovery and permanent disability.
What’s the Difference Between Ischemic and Hemorrhagic Strokes?
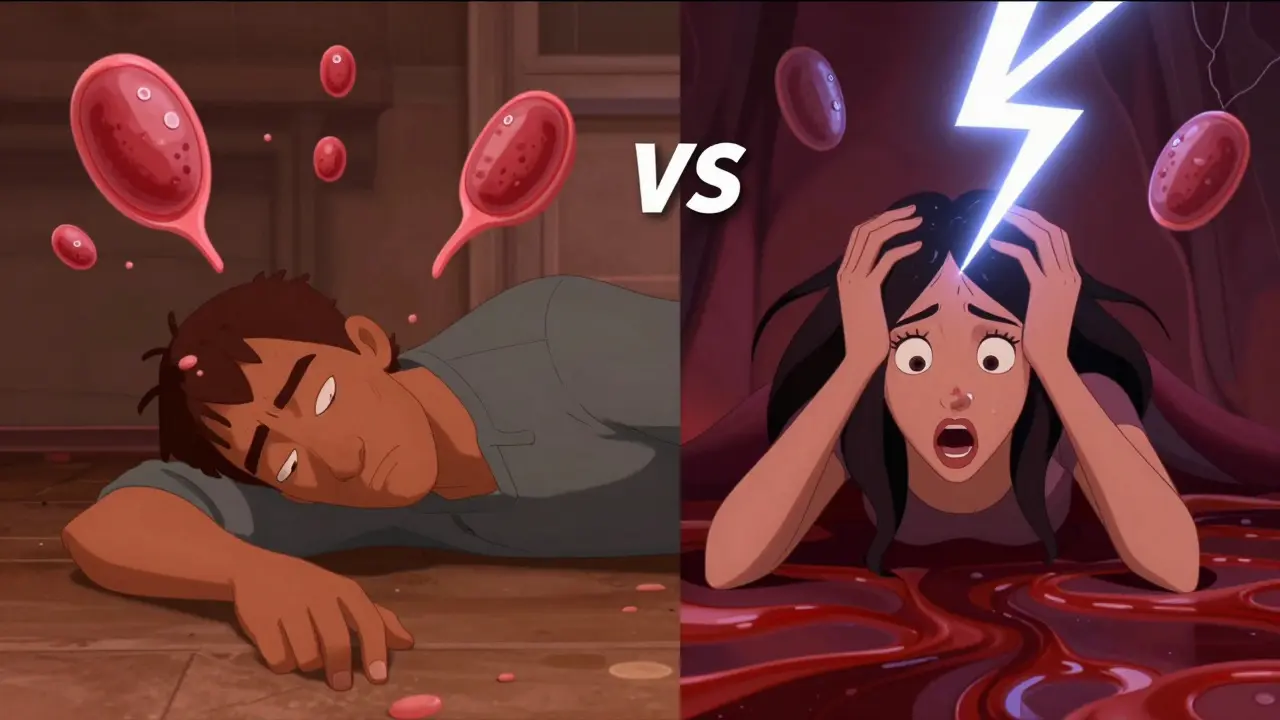
Think of your brain like a city. It needs constant power - blood flow - to keep everything running. When that power gets cut off, it’s an ischemic stroke. When a pipe bursts and floods the streets, it’s a hemorrhagic stroke. One blocks, the other bleeds.
Ischemic strokes make up about 87% of all strokes. They happen when a clot blocks an artery leading to your brain. The clot might form right there in your brain (thrombotic), or travel from your heart or neck (embolic). In some cases, doctors can’t find the cause - those are called cryptogenic strokes, and they’re surprisingly common, making up about 30% of ischemic cases.
Hemorrhagic strokes are less common - just 13-15% of cases - but often more deadly. These happen when a blood vessel in or around your brain bursts. There are two main kinds: intracerebral hemorrhage (bleeding inside the brain tissue) and subarachnoid hemorrhage (bleeding on the brain’s surface, often from a ruptured aneurysm). These aren’t slow burns. They’re explosions. A sudden, severe headache - the worst you’ve ever felt - is a classic sign.
How Do the Symptoms Differ?
Both types can cause sudden numbness, trouble speaking, or weakness on one side of your body. But hemorrhagic strokes often come with wild, unmistakable signs that ischemic strokes rarely do.
Here’s what sets them apart:
- Headache: 92% of hemorrhagic stroke patients report a thunderclap headache - like being hit in the head with a hammer. Only 19% of ischemic stroke patients do.
- Seizures: Happen in nearly 1 in 6 hemorrhagic strokes. Almost never in ischemic ones.
- Eye and pupil changes: Dilated pupils, unequal pupils, or trouble moving your eyes? That’s far more common in bleeding strokes.
- Agitation: Over 79% of hemorrhagic stroke patients become confused or agitated. Only 7% of ischemic patients do.
Ischemic strokes often creep in. You might notice your arm feels heavy, then your speech gets slurred, then your face droops - over 10 to 30 minutes. Hemorrhagic strokes hit like a lightning bolt. One moment you’re fine. The next, you’re on the floor, screaming from pain.
What Causes Each Type?
Understanding the cause helps you prevent it.
Ischemic strokes are tied to heart and artery problems:
- Atrial fibrillation (AFib): This irregular heartbeat lets blood pool and clot in your heart. If that clot breaks loose, it can travel to your brain. AFib increases your stroke risk by 500%.
- Atherosclerosis: Fatty buildup in your carotid or brain arteries can block blood flow. This is the most common cause of thrombotic strokes.
- High cholesterol and smoking: Both damage your arteries and make clots more likely.
Hemorrhagic strokes are mostly about pressure:
- Uncontrolled high blood pressure: This is the #1 cause. About 80% of intracerebral hemorrhages happen because decades of high blood pressure weakened small brain arteries until they burst.
- Aneurysms: Weak spots in artery walls that balloon out. If one ruptures, it causes a subarachnoid hemorrhage.
- Bleeding disorders or anticoagulant overuse: Blood thinners can turn a minor bleed into a disaster if not monitored.
How Are They Treated?
Time is brain - but the clock ticks differently for each stroke type.
For ischemic strokes, doctors try to dissolve or remove the clot fast:
- tPA (alteplase) or tenecteplase: Clot-busting drugs given through an IV. Must be given within 3-4.5 hours of symptom onset.
- Thrombectomy: A catheter is threaded up from the groin to physically pull the clot out. Works up to 24 hours after symptoms start - if the brain tissue is still salvageable.
Hemorrhagic strokes are treated by stopping the bleeding and reducing pressure:
- Coiling or clipping: For aneurysms, doctors either insert tiny coils via a catheter (coiling) or place a metal clip on the aneurysm neck (clipping) to stop blood flow into it.
- Draining blood: In some cases, surgeons use minimally invasive tools to suction out pooled blood and reduce pressure on the brain.
- Medications: Drugs to lower blood pressure, prevent seizures, or reduce brain swelling.
First thing in the ER? A CT scan. It shows if there’s bleeding - and it’s the only way to know whether to give clot-busting drugs. Giving tPA to someone with a hemorrhagic stroke could kill them.
How to Prevent Strokes - Type by Type
You can’t stop every stroke, but you can slash your risk - big time.
For ischemic stroke prevention:
- Treat AFib: If you have atrial fibrillation, take your blood thinner - warfarin, apixaban, rivaroxaban - exactly as prescribed. Studies show these reduce stroke risk by 60-70%.
- Take aspirin or clopidogrel: If you’ve had a prior stroke or TIA, daily low-dose aspirin (81 mg) or clopidogrel cuts your risk of another stroke by 25%.
- Lower cholesterol: Statins don’t just protect your heart - they stabilize plaque in your arteries, reducing clot risk.
- Quit smoking: Within one year of quitting, your stroke risk drops by half.
For hemorrhagic stroke prevention:
- Control your blood pressure: This is the single most powerful thing you can do. The SPRINT trial showed that keeping systolic pressure below 120 mmHg - not 140 - cuts hemorrhagic stroke risk by 38%.
- Check for aneurysms: If you have a family history of ruptured aneurysms or have polycystic kidney disease, ask your doctor about screening. Not everyone needs it, but some do.
- Use blood thinners wisely: If you’re on anticoagulants, get regular blood tests. Don’t mix them with NSAIDs like ibuprofen unless your doctor says it’s safe.
For both types:
- Eat a Mediterranean diet: Lots of vegetables, olive oil, fish, nuts, and whole grains. The PREDIMED study showed a 30% lower stroke risk.
- Move every day: 150 minutes of brisk walking a week cuts overall stroke risk by 27%.
- Limit alcohol: More than one drink a day raises your risk. Two drinks a day? That’s a 50% higher chance of hemorrhagic stroke.

What Happens After a Stroke?
Recovery isn’t the same for everyone. A 2022 meta-analysis found hemorrhagic stroke patients had a 23% higher 30-day death rate than ischemic patients - even when severity was matched. But long-term outcomes? That’s more about how much brain tissue was damaged, not just the type.
Survivors of ischemic strokes often regain function with rehab - speech therapy, physical therapy, occupational therapy. Many return to work. Hemorrhagic stroke survivors face a longer, harder road. Swelling and pressure can cause more widespread damage. But recovery is still possible - especially with early, intensive rehab.
The biggest predictor of outcome? Getting help fast. In patient stories, 73% who had good recoveries said they recognized the FAST signs (Face drooping, Arm weakness, Speech difficulty, Time to call 911) within five minutes.
What’s New in Stroke Care?
Science is moving fast.
For ischemic strokes, MRI scans are now being used to find patients who might still benefit from tPA up to 9 hours after symptoms start - a big leap from the old 4.5-hour window. In Australia, telestroke networks are bringing specialist care to rural towns in real time.
For hemorrhagic strokes, a 2022 trial showed that using a minimally invasive technique with clot-dissolving drugs reduced death rates by 10% at one year.
And soon, a simple blood test might tell paramedics within minutes whether a stroke is ischemic or hemorrhagic. A biomarker called GFAP is showing 92% accuracy. That could mean faster, safer treatment - even before reaching the hospital.
Don’t Wait. Act Now.
Strokes don’t care if you’re young, fit, or healthy. They strike without warning. But you’re not powerless.
If you have high blood pressure - get it under control. If you have AFib - take your meds. If you smoke - quit today. If you’re over 55 - get checked for carotid artery disease. If you’ve had a TIA - that’s your body’s final warning. Don’t ignore it.
Know the signs. Know your risk. And if you or someone else shows even one symptom - call emergency services immediately. Don’t wait. Don’t drive yourself. Don’t hope it’ll pass. Every minute counts.


Man, I just read this whole thing and I’m fired up. Every single person over 40 needs to bookmark this. I had my uncle go through an ischemic stroke last year - he was fine until he couldn’t lift his coffee cup, and we thought he was just being lazy. Turns out, it was a tiny clot in his left MCA. If we’d known about the FAST signs earlier, he wouldn’t have lost three months of speech therapy. Don’t wait for the thunderclap headache - sometimes the warning is just your arm feeling like it’s wrapped in wet concrete. Get checked. Take your meds. Quit smoking. Your future self will thank you. I’m telling my whole family this link tonight.
87% ischemic? That’s statistically insignificant if you’re not in a high-risk cohort. The real issue is the overmedicalization of prevention. Statins for everyone? Aspirin as a daily tonic? This is Big Pharma’s playbook. Hemorrhagic strokes are often genetic - you can’t control aneurysms with kale smoothies. And let’s not pretend a CT scan is foolproof. I’ve seen false negatives. The real solution? Stop treating stroke like a software bug you can patch with drugs. It’s a systemic failure of vascular integrity - and the system is rigged.
ok so i just cried reading this 😭 like… i lost my mom to a hemorrhagic stroke and she had NO high bp, no aneurysm history, just… woke up screaming and then it was over. i hate how people act like if you just ‘took care of yourself’ it wouldn’t happen. what about the 20 year olds? the ones with no risk factors? the ones who just… got unlucky? this article feels like victim-blaming with footnotes. 🤕💔
Interesting breakdown, but I’m curious about the cryptogenic ischemic strokes - 30% of cases with no identifiable cause. That’s a massive blind spot. Are we missing something in diagnostics? Could gut microbiome dysbiosis play a role in clot formation? Or maybe chronic low-grade inflammation from environmental toxins? The current model feels incomplete. We focus so hard on the ‘how’ of clotting or bleeding that we ignore the ‘why’ behind the vulnerability. Maybe the real prevention isn’t just controlling BP or AFib - maybe it’s rethinking how we live, eat, and stress. What if the answer isn’t in the artery… but in the lifestyle?
Stop pushing meds like they’re candy. You think taking aspirin makes you invincible? Newsflash: it doesn’t. And that ‘Mediterranean diet’ thing? That’s just a fancy way of saying eat less crap. Also - why is every study cited from the US? What about global data? Most strokes happen in low-income countries where no one has access to CT scans or tPA. You’re preaching to the choir who can afford to care. Meanwhile, the rest of the world is just hoping they don’t collapse in the middle of the field. And don’t get me started on telestroke networks - nice for suburbs, useless in Appalachia.
Ugh. Another article telling me I’m doomed if I don’t take a pill. I’m 38, I eat clean, I walk 10k steps a day, I don’t drink, I don’t smoke - and I still have anxiety every time my head hurts. Why? Because everyone makes stroke sound like a moral failure. Like if you just tried harder you wouldn’t get it. But what if your body is just broken? What if you inherited bad genes? What if you’re not the problem - the system is? I’m tired of being guilt-tripped into becoming a perfect human just to avoid dying.
The American medical-industrial complex has weaponized stroke awareness into a moral crusade. We are told to control our BP, take our statins, eat our quinoa - as if stroke is a failure of individual discipline. But consider this: the same nation that sells you kale smoothies also sells you fast food, soda, and stress. We have created a society where the average citizen is chronically inflamed, chronically sedentary, and chronically anxious - then we blame them for the consequences. The real epidemic is not stroke - it is systemic neglect. The solution? Not more pills. Not more apps. Not more guilt. A societal reset. A return to community, to movement, to rest - not pharmaceutical control.
There’s a beautiful paradox here. We treat stroke like an enemy to be defeated - with drugs, scans, and surgical interventions. But what if stroke isn’t an attack, but a signal? A final cry from a body that’s been ignored for decades. The clot isn’t just a blockage - it’s the accumulation of silence. The bleed isn’t just a rupture - it’s the collapse of suppressed stress, poor sleep, emotional isolation. We fix the artery, but we never fix the life. Maybe the most powerful prevention isn’t a CT scan or a blood thinner - it’s learning to listen. To your body. To your heart. To the quiet voice that says, ‘I’m tired.’
This is such a beautiful and clear explanation! I’m from India and we don’t talk enough about strokes here - people think it’s only for old folks. My aunt had a mini-stroke last year and we didn’t know what was happening until she couldn’t say ‘chai’ properly. Now I’ve shared this with my whole family. I told my dad to get his BP checked every month and my sister to stop skipping meals. Small steps, but they matter. And yes, the Mediterranean diet? We already have it here - dal, rice, spinach, turmeric, nuts. We just call it ‘normal food’. 😊
Bro. My uncle died from hemorrhagic stroke at 52. No warning. Just collapsed at the temple. They said his BP was 220/110. But he never felt sick. Never had headaches. That’s the scariest part - you feel fine until you’re not. Don’t wait for symptoms. Get checked. Even if you think you’re fine. Just once. Please.
So let me get this straight - we’re supposed to believe a blood test can tell if it’s ischemic or hemorrhagic before you even hit the ER? That’s like saying we’ll have a ‘cancer detector’ in our smartwatches next. 🤨 Also, who wrote this? A pharmaceutical rep with a thesaurus? ‘Thunderclap headache’? ‘Explosions’? ‘Cryptogenic’? You’re not educating people - you’re performing a TED Talk. Real people don’t talk like this. Just tell us: check your BP. Take your meds. Don’t smoke. Call 911. Done.
It is imperative to emphasize that the pathophysiological mechanisms underlying ischemic and hemorrhagic strokes are fundamentally divergent and necessitate distinct clinical protocols. The utilization of thrombolytic agents in the presence of intracranial hemorrhage constitutes a contraindication of the highest order, as it may precipitate catastrophic hemorrhagic transformation. Furthermore, the epidemiological distribution of stroke subtypes varies significantly across genetic and environmental strata, thereby necessitating region-specific preventive paradigms. The assertion that dietary modification alone can mitigate risk is an oversimplification that disregards the multifactorial etiology of cerebrovascular disease.
Yeah, this is solid info. I work in a rural clinic and we get stroke cases all the time - usually too late. People wait because they don’t know the signs, or they’re scared of the hospital, or they think it’ll pass. I’ve had patients say ‘I just need to sleep it off.’ I show them the FAST acronym on my phone. One guy said ‘I didn’t know my face was drooping till my wife pointed it out.’ Honestly? Just knowing the signs saves lives. No fancy tech needed. Just awareness. And a quick call.
GFAP biomarker? 92% accuracy? That’s a lie. They’ve been testing this since 2018. It’s never been validated in large populations. And why is no one talking about the fact that 70% of stroke patients are on Medicaid or uninsured? This whole article is a distraction. The real issue is the healthcare system. They want you to think you can fix this with diet and pills - while the system lets people die because they can’t afford a CT scan. This isn’t prevention - it’s propaganda.
bro i had a stroke at 29. no high bp, no smoking, no family history. just woke up with a headache and couldn’t hold my phone. they said it was cryptogenic. i still don’t know why. now i take 4 pills a day and i’m scared to drive. this article makes it sound like it’s all your fault. it’s not. it’s just… luck. bad luck. and now i’m stuck with it.