Chronic Diarrhea: Causes, Management, and What Works
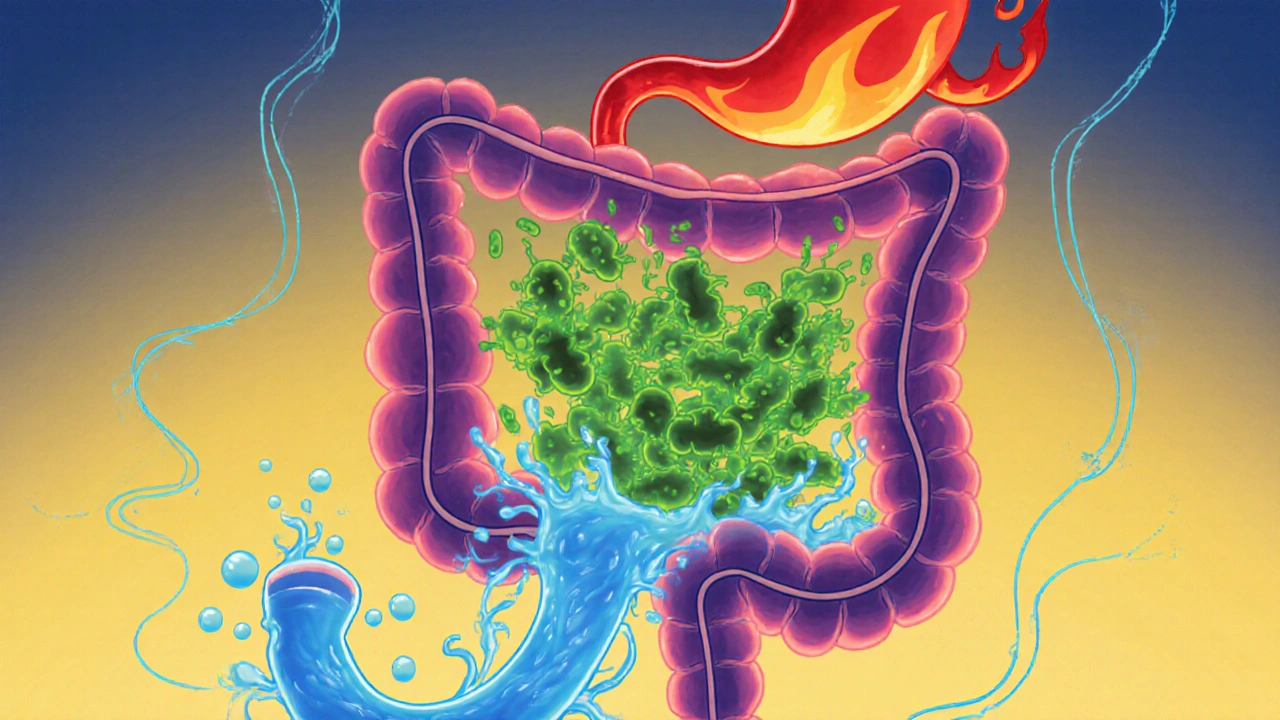
When you’ve had loose stools for more than four weeks, you’re dealing with chronic diarrhea, a persistent digestive issue that lasts longer than four weeks and often signals an underlying condition. Also known as persistent diarrhea, it’s not just an annoying day-to-day problem—it can drain your energy, disrupt your sleep, and even affect your mental health. Unlike short-term bouts from food poisoning or a virus, chronic diarrhea sticks around because something in your system isn’t working right. It could be your gut bacteria, how your body absorbs nutrients, or even a reaction to a medication you’ve been taking for months.
Many people with chronic diarrhea don’t realize it’s linked to conditions like irritable bowel syndrome, a common functional disorder that alters how the gut moves and senses pain, or Crohn’s disease, an inflammatory bowel condition that attacks the digestive tract. Others find out their symptoms started after antibiotics wiped out good bacteria, or because of a food intolerance they never tested for—like lactose or gluten. Even some heart meds, diabetes drugs, or painkillers can cause it as a side effect. You won’t find this in every doctor’s office, but studies show over 30% of chronic diarrhea cases are tied to medication use.
What you do next matters more than you think. Simply popping anti-diarrhea pills won’t fix the root cause. Tracking what you eat, how you feel, and what meds you’re on can point you toward answers. Some people find relief by adjusting their fiber intake, others need a stool test to check for infections like C. diff, and a few discover their symptoms vanished after switching a prescription. The good news? You’re not alone. The posts below cover real stories and science-backed approaches—from how medication adherence plays a role in triggering or worsening symptoms, to how gut health, the balance of microbes in your digestive tract that affects everything from digestion to immunity can be rebuilt. You’ll also find guides on how to spot when a drug is to blame, how to manage symptoms without relying on quick fixes, and what tests actually matter. This isn’t about guesswork. It’s about connecting the dots between what you take, what you eat, and why your body reacts the way it does.