Osteoporosis — what it is and what you can do today
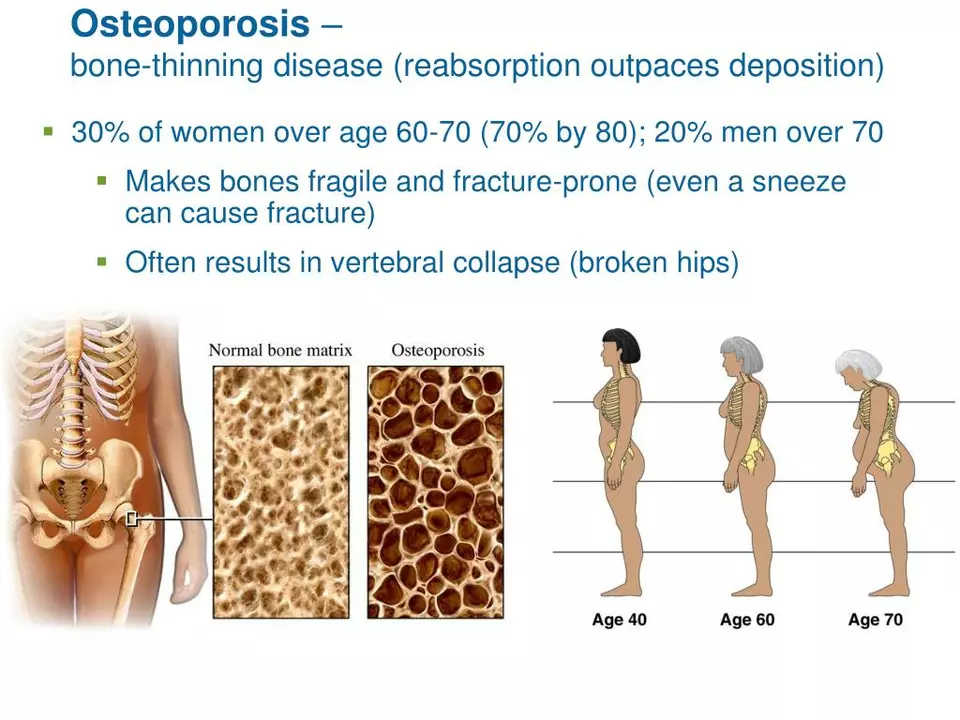
Did you know one in three women and one in five men over 50 will break a bone because of osteoporosis? That makes bone health a top priority once you hit middle age. Osteoporosis means your bones lose density and strength, which raises fracture risk. The good news: small, practical changes plus the right medical care cut that risk a lot.
How it's diagnosed
Your doctor will usually order a DEXA (bone density) scan. The result is a T-score: normal is above -1.0, osteopenia is between -1.0 and -2.5, and osteoporosis is -2.5 or lower. Doctors may also use the FRAX tool to estimate your 10-year fracture risk. If you’ve already had a low-trauma fracture (like a hip or wrist from a simple fall), that’s treated as a red flag regardless of score.
Practical steps to protect and strengthen bones
Diet and supplements: aim for about 1,000–1,200 mg of calcium a day (from food first: dairy, leafy greens, fortified foods). Vitamin D helps your body use calcium — a common target is 800–1,000 IU daily, but your doctor may check your blood level and adjust the dose.
Exercise: do weight-bearing activity (walking, hiking, dancing) most days and add strength training 2–3 times a week. Balance and mobility work — like tai chi or simple heel-to-toe walks — lowers fall risk and prevents fractures.
Lifestyle changes: quit smoking and limit alcohol (keep it to a drink or two a day max). Make your home safer: remove loose rugs, add good lighting, and install grab bars where needed.
Medications: if your fracture risk is high, prescription treatment can dramatically reduce fractures. Common first-line drugs are oral bisphosphonates (alendronate, risedronate). They’re effective but need to be taken exactly as directed to avoid stomach or esophageal irritation. Other options include denosumab (an injection every 6 months), raloxifene for some postmenopausal women, and anabolic agents like teriparatide for severe cases. Each has pros and cons — for example, rare risks include osteonecrosis of the jaw with some drugs, so dental checks and medical follow-up matter.
Monitoring: repeat DEXA scans are usually scheduled every 1–2 years depending on treatment and risk. Your doctor will also track side effects and decide when to pause or switch therapy.
When to see a doctor right away: if you’ve had a fall, notice a sudden back pain (possible vertebral fracture), or have risk factors like long-term steroid use, early menopause, low body weight, or a strong family history of hip fractures.
Want a simple start? Book a DEXA if you’re over 65 (women) or 70 (men) or sooner with risk factors. Add a short daily walk, check your calcium and vitamin D, and talk with your doctor about fracture risk. Small, steady steps add up to stronger bones and fewer trips to the ER.