Treatment Matchmaker
Find Your Best Provera Alternative
Answer a few questions about your condition and priorities to see which treatment options might work best for you.
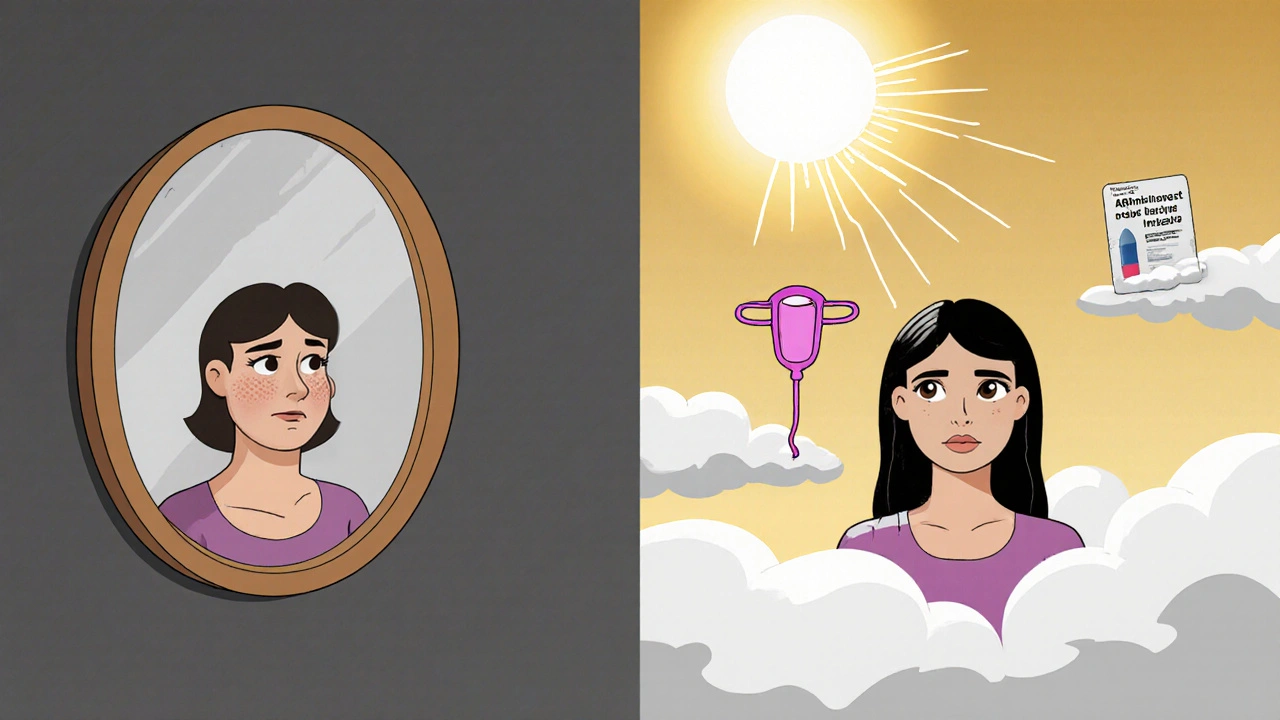
When your body doesn’t regulate periods the way it should, or when you’re trying to manage endometriosis, PCOS, or abnormal bleeding, your doctor might suggest Provera - the brand name for medroxyprogesterone. It’s a synthetic hormone that mimics progesterone, one of your body’s natural female hormones. But it’s not the only option. Many women wonder: is there something better? Safer? More effective? The truth is, Provera works for some, but it’s not the right fit for everyone. Let’s look at what else is out there - and what actually makes a difference in real life.
What Provera Actually Does
Provera (medroxyprogesterone acetate) is a progestin. It doesn’t contain estrogen. That makes it useful for women who can’t take estrogen - maybe because of blood clot risks, migraines with aura, or a history of breast cancer. It’s often prescribed to trigger a period in women who haven’t had one in months, to thin the uterine lining in cases of abnormal bleeding, or to manage symptoms of endometriosis. It’s also used in some forms of birth control, though usually in combination with estrogen.
Most people take it orally, once a day for 5 to 10 days. In about 70% of cases, a withdrawal bleed happens within a week after stopping. That’s how doctors know the lining was thick enough to shed. But it doesn’t prevent ovulation like birth control pills do. So if you’re using it for cycle control, you still need another method if you’re trying to avoid pregnancy.
Common Side Effects of Provera
Provera isn’t gentle. Many women report weight gain, bloating, breast tenderness, mood swings, and headaches. Some feel dizzy or fatigued. A small number report depression or anxiety worsening. These aren’t rare - they’re common enough that doctors often warn patients before prescribing. Long-term use can also lower bone density, especially if taken for more than two years without estrogen. That’s why it’s not usually recommended for ongoing hormone replacement in menopausal women unless combined with estrogen.
One thing people don’t talk about enough: Provera can cause spotting between periods. For women already dealing with irregular bleeding, that’s frustrating. It can feel like the treatment is making things worse before they get better.
Alternative 1: Norethindrone (Aygestin, Norlutate)
Norethindrone is another progestin, but it’s slightly different in how it acts on the body. Like Provera, it’s used to regulate periods, treat endometriosis, and stop abnormal bleeding. But it’s often better tolerated. Many women report less bloating and mood disruption with norethindrone. It’s also used in some combined birth control pills, which means it’s been tested in longer-term use.
One key difference: norethindrone can be taken daily for longer periods without needing to stop and wait for a bleed. That’s useful if you want continuous cycle control without monthly withdrawal bleeds. It’s also more commonly used in lower doses for endometriosis management. Studies show similar effectiveness to Provera, but with fewer reports of weight gain and emotional side effects.
Alternative 2: Levonorgestrel IUD (Mirena, Liletta)
If you’re looking for a long-term, low-maintenance option, the levonorgestrel IUD is hard to beat. It releases a small amount of progestin directly into the uterus - so your body doesn’t get a full-body dose. That means fewer systemic side effects. Many women using Mirena or Liletta see their periods get lighter, then stop entirely within six to twelve months.
It’s FDA-approved for heavy menstrual bleeding and endometriosis. In one study, 90% of women with abnormal uterine bleeding had significant improvement after one year. And because it lasts up to eight years, you don’t have to remember a daily pill. The downside? Insertion can be uncomfortable, and some women report cramping or spotting in the first few months. But for those who stick with it, the results are often life-changing.

Alternative 3: Combined Oral Contraceptives (COCs)
Birth control pills that contain both estrogen and progestin - like Loestrin, Yaz, or Alesse - are often prescribed for menstrual regulation. They work by suppressing ovulation and stabilizing the uterine lining. Unlike Provera, they provide consistent hormone levels every day, which means fewer spikes and crashes that lead to mood swings or breakthrough bleeding.
They’re especially helpful for women with PCOS, where irregular periods are tied to high androgens and insulin resistance. COCs can reduce acne, excess hair growth, and cycle unpredictability. But they’re not for everyone. If you have a history of blood clots, high blood pressure, migraines with aura, or are over 35 and smoke, estrogen isn’t safe. That’s where Provera or progestin-only options come in.
Alternative 4: Dienogest (Visanne)
Dienogest is a newer progestin that’s specifically designed for endometriosis. It’s not available everywhere - in the U.S., it’s not FDA-approved, but it’s widely used in Europe and Australia. In Australia, it’s prescribed off-label for endometriosis and heavy bleeding. Unlike Provera, dienogest works continuously, without requiring a break. It reduces inflammation in endometrial tissue and shrinks lesions.
Studies show it’s more effective than Provera at reducing pelvic pain and improving quality of life in endometriosis patients. Side effects are similar - acne, headaches, mood changes - but many women report less weight gain. It’s taken daily, and you don’t get monthly bleeds. That’s a plus for some, a minus for others who prefer regular periods.
Alternative 5: GnRH Agonists (Lupron, Synarel)
If you’ve tried everything else and still have severe endometriosis or heavy bleeding, your doctor might suggest a GnRH agonist. These drugs temporarily shut down ovarian hormone production, putting you into a temporary, reversible menopause. That means no estrogen, no progesterone - and no endometrial growth.
They’re powerful. Many women see dramatic pain relief within weeks. But the side effects are intense: hot flashes, bone loss, vaginal dryness, insomnia. They’re usually limited to 6 months because of the risk of osteoporosis. Often, they’re used as a bridge - to shrink tissue before surgery, or to test if surgery will help. They’re not a long-term solution, but they can reset the system when other options fail.
Non-Hormonal Options
Not everyone wants hormones. For those who don’t, there are other paths. Tranexamic acid (Lysteda) reduces bleeding by helping blood clot. It’s taken only during your period - no daily pills. NSAIDs like ibuprofen can cut heavy flow by up to 50% by reducing prostaglandins. Both are safe for short-term use and don’t affect your hormones.
For long-term management, the copper IUD (Paragard) doesn’t help with bleeding - it often makes it worse. But it’s hormone-free and lasts 10 years. If you’re looking for contraception without hormones, it’s an option. Just know: it won’t fix your bleeding.
Choosing the Right Option for You
There’s no one-size-fits-all. Your choice depends on your goals:
- If you want quick period control and can’t take estrogen, Provera or norethindrone are good starters.
- If you want long-term relief without daily pills, the levonorgestrel IUD is the most effective.
- If you have PCOS or acne, combined birth control pills often help more than Provera alone.
- If you have severe endometriosis, dienogest or GnRH agonists may be better than Provera.
- If you want no hormones at all, tranexamic acid or NSAIDs can reduce bleeding.
Also consider your tolerance for side effects. Provera is cheap and widely available, but if you’ve had bad reactions before, it’s worth trying something else. Many women switch from Provera to the IUD and wonder why they didn’t do it sooner.
What Doctors Don’t Always Tell You
Provera is often the first option because it’s inexpensive and familiar. But it’s not the best for everyone. Some doctors don’t know about dienogest or how effective the IUD is for bleeding. Others assume you’ll tolerate side effects because "it’s just a pill." But if you’re feeling depressed, gaining weight, or spotting constantly, that’s not normal - it’s a sign the treatment isn’t right.
Ask your doctor: "What’s the goal here? To stop bleeding? To prevent pregnancy? To manage pain?" Then ask: "What are the alternatives? What have other women with my condition found works best?" Don’t settle for the first option. You deserve to feel better, not just have a period.
When to See a Specialist
If you’ve tried Provera and at least one other option without success, it’s time to see a gynecologist who specializes in menstrual disorders or endometriosis. These doctors know about newer treatments, hormonal options, and non-hormonal strategies that general practitioners might overlook. They can order pelvic ultrasounds, check for adenomyosis, or test for thyroid issues that mimic hormonal imbalance.
Don’t wait years thinking "this is just how it is." Abnormal bleeding, severe pain, and missed periods are signs your body needs help - not just masking.
Can Provera cause weight gain?
Yes, weight gain is a common side effect of Provera. Many women report gaining 5 to 10 pounds, mostly from water retention and increased appetite. This isn’t true fat gain for everyone, but it’s frequent enough that doctors warn about it. Alternatives like the levonorgestrel IUD or dienogest are less likely to cause this.
Is Provera the same as birth control?
No. Provera is a progestin-only medication used to regulate periods or treat bleeding, but it doesn’t reliably prevent ovulation. Birth control pills usually combine estrogen and progestin to stop ovulation completely. If you need contraception, you’ll need another method while taking Provera.
Can I take Provera long-term?
It’s not recommended. Long-term use (over 2 years) can lower bone density and increase fracture risk, especially without estrogen. It’s meant for short-term use - like triggering a period or managing bleeding episodes. For ongoing treatment, alternatives like the IUD or dienogest are safer.
Does Provera help with PCOS?
It can help regulate periods in women with PCOS, but it doesn’t address the root causes like insulin resistance or high androgens. Combined birth control pills are often more effective because they lower testosterone and improve acne and hair growth. Provera alone won’t fix those symptoms.
What’s the best alternative to Provera for endometriosis?
In Australia and Europe, dienogest (Visanne) is considered the gold standard for endometriosis because it reduces lesions and pain with fewer side effects than Provera. In the U.S., the levonorgestrel IUD is often the first choice due to its effectiveness and long-term use. GnRH agonists work well for severe cases but are only for short-term use.


Provera is just the beginning. Big Pharma pushes it because it’s cheap and patent-free. Meanwhile, they’re hiding the real solutions - like dienogest - that work better but cost more. You think this is medicine? It’s a cash grab.
They don’t want you to know about the IUD either. Too many women get cured and stop buying pills. That’s not a coincidence.
OMG I took provera for 3 months and i started seeing shadows in the corner of my room and my cat stopped talking to me like literally she just stared and walked away
and then i found out my doctor got paid by the pharma rep to prescribe it i swear to god they are all in on it
the iud is the real villain too they put nano chips in them to track your emotions i read it on a forum
Oh sweetie. You think Provera is the problem? Honey, the real villain is the medical system that treats women’s pain like a suggestion.
"Just take a pill." "It’s probably stress." "Maybe you’re just hormonal."
Meanwhile, men get MRIs for headaches. Women get Provera.
At least the IUD gives you back your life. Even if it’s just a temporary truce with your body.
Provera made me cry in the grocery store over a bag of chips. I was 27. I didn’t even like chips. That’s not side effects - that’s a soul violation.
I switched to the Mirena and now I don’t bleed at all. No more pads. No more panic. No more pretending I’m fine.
Why did I wait 4 years? Because my doctor said "it’s normal." It’s not normal. It’s torture dressed up as treatment.
It is imperative to recognize that the pharmacological landscape of hormonal regulation for gynecological conditions is both complex and deeply individualized. While Provera remains a widely utilized and cost-effective intervention, its long-term use must be carefully weighed against potential adverse effects on bone mineral density, particularly in the absence of concomitant estrogen therapy.
Conversely, the levonorgestrel-releasing intrauterine device offers a paradigm shift in therapeutic delivery - localized, sustained, and minimally systemic. Clinical evidence supports its efficacy in reducing menorrhagia by upwards of 90% over a 12-month period, with significantly improved patient satisfaction metrics compared to oral progestins.
Furthermore, dienogest, though not yet FDA-approved in the United States, has demonstrated superior lesion regression in endometriosis patients in multiple randomized controlled trials conducted in European jurisdictions. Its continuous administration profile eliminates the artificial withdrawal bleeds inherent to cyclic progestin regimens, thereby enhancing quality of life.
It is therefore not merely a question of efficacy, but of personalized therapeutic alignment: the goal must be symptom resolution, not merely cycle induction. A multidisciplinary approach involving endocrinology, reproductive endocrinology, and patient-reported outcome measures is essential for optimal management.
Ugh. This post is just a long ad for IUDs. Everyone knows Provera works fine if you just stop being dramatic.
My cousin took it for 2 years and she’s fine. You just need to man up and deal with a little bloating.
Also, why are you all obsessed with hormones? Just eat less sugar and pray. That’s what my grandma did.
Provera is a trap. You think you’re getting help but you’re just being medicated into silence.
Women have been gaslit for centuries. This is just the latest version.
Hey, I was in your shoes. Took Provera, cried for a week, gained 8 lbs, felt like a zombie.
I switched to the Mirena. First 3 months? Messy. Cramps. Spotting. Felt like my body was in rebellion.
Then? Magic. No more panic attacks before my period. No more hiding pads. No more wondering if I’m broken.
It’s not perfect. But it’s freedom. And you deserve that. Don’t settle for "it’s just how it is."
Wow. So much effort for something that’s just your body being a bitch.
I had PCOS. Took pills. Got the IUD. Still bled. Then I just stopped caring. Life went on.
Stop overcomplicating it. You’re not broken. You’re just a woman. Deal.
Provera? Please. That’s what they give you when they don’t wanna do the work.
I’ve seen 7 gynecologists. Every single one pushed Provera first. Then when I asked about dienogest? Blank stares. One said, "That’s not FDA approved, so we don’t use it."
Translation: I don’t know what you’re talking about, and I’m not gonna look it up.
And don’t even get me started on the IUD. My last doctor said, "It’s for girls who want to be promiscuous." I walked out.
Women’s health is a joke. And you’re all just sitting here reading about it instead of demanding better.
Thank you for this comprehensive overview. As a clinician, I appreciate the balanced presentation of both hormonal and non-hormonal options. The emphasis on patient autonomy and individualized care is particularly commendable.
It is worth noting that while the levonorgestrel IUD is indeed the most effective long-term solution for abnormal uterine bleeding, patient preference and anatomical factors - such as uterine fibroids or congenital anomalies - may preclude its use.
Additionally, access to dienogest remains a significant barrier in the United States, despite its proven efficacy. Advocacy for FDA approval and insurance coverage is urgently needed.
For patients seeking non-hormonal alternatives, tranexamic acid remains underutilized and should be considered earlier in the treatment algorithm, especially for those with heavy menstrual bleeding and contraindications to hormonal therapy.
Continued dialogue between patients and providers, grounded in evidence and empathy, remains the cornerstone of optimal gynecologic care.