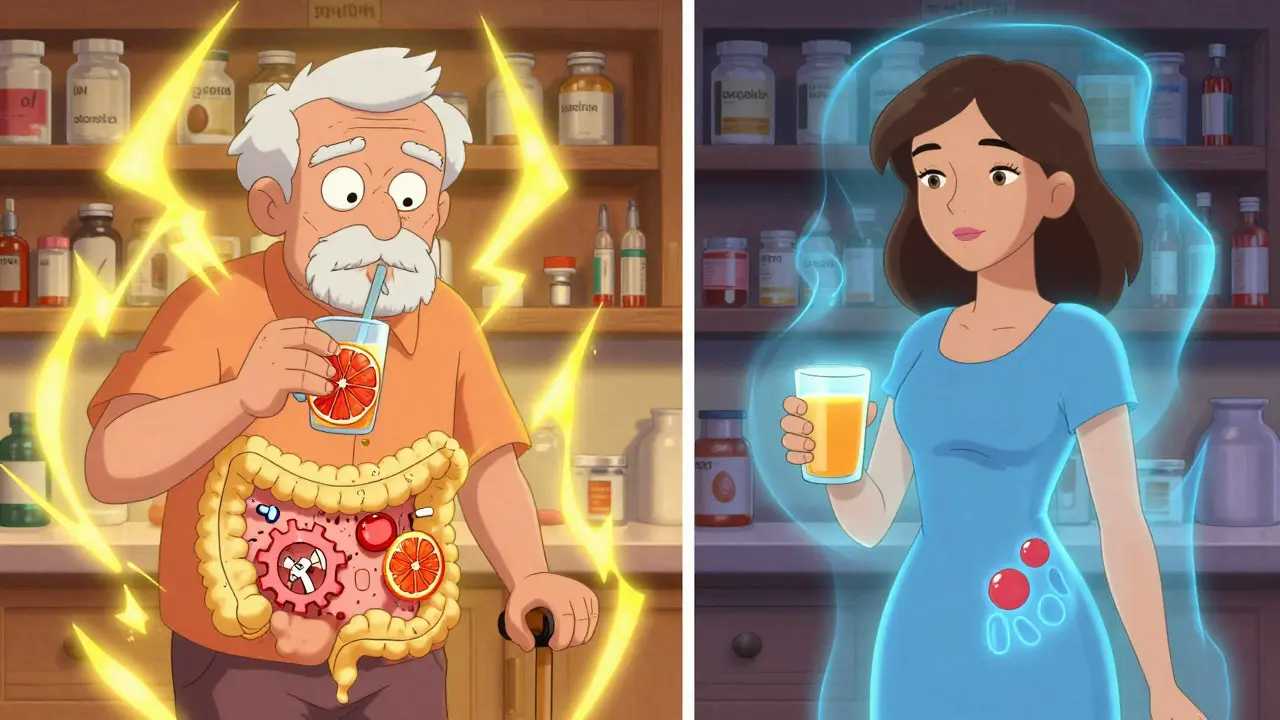
When you take warfarin for a blood clot or an SSRI for depression, you might not think about your morning glass of grapefruit juice. But that juice could be quietly changing how your meds work - and not in a good way. The problem lies in something called the CYP450 system, a group of liver and gut enzymes that break down over 75% of all prescription drugs. Grapefruit doesn’t just add flavor to your breakfast; it can shut down key parts of this system, leading to dangerous drug buildup in your body.
How Grapefruit Disrupts Drug Metabolism
Grapefruit isn’t just a fruit - it’s a chemical disruptor. Inside it are compounds called furanocoumarins, mainly bergamottin and DHB. These don’t just block enzymes temporarily; they permanently damage them. Once you drink grapefruit juice, these compounds bind to CYP3A4 enzymes in your gut wall, wrecking them so they can’t break down drugs anymore. Your body doesn’t just flush them out - it has to make brand-new enzymes, which takes days.
That’s why timing doesn’t help. Drinking grapefruit juice at breakfast and taking your pill at dinner? Still risky. The damage lasts 24 to 72 hours. Even a single 8-ounce glass can knock down CYP3A4 activity by nearly half, according to studies from the American Academy of Family Physicians. And it’s not just CYP3A4 - grapefruit also messes with CYP2C9, CYP2D6, and others. This broad effect makes it one of the most dangerous food-drug interactions out there.
Warfarin and Grapefruit: A Quiet Danger
Warfarin is a blood thinner with a razor-thin safety margin. Too little, and you risk a clot. Too much, and you could bleed internally. About 85% of warfarin is broken down by CYP2C9, with the rest handled by CYP3A4. Grapefruit’s furanocoumarins inhibit both enzymes, so there’s a real risk - even if it’s not as strong as with other drugs.
Studies show mixed results. Some patients see their INR (a measure of blood clotting time) jump 15-25% after drinking grapefruit juice. Others show no change. Why? Genetics. People with CYP2C9*2 or *3 gene variants break down warfarin slower to begin with. For them, grapefruit can be the tipping point. The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends avoiding grapefruit entirely if you have these variants. Genetic testing for these variants costs $250-$400, and it’s worth it if you’re on warfarin long-term.
Real-world data backs this up. A Drugs.com analysis found 8.7% of warfarin users specifically avoid grapefruit - far more than SSRI users. Reddit users on r/pharmacy reported 32% of those who accidentally mixed grapefruit with warfarin saw their INR go out of range. One man in Ohio had to be hospitalized after a week of daily grapefruit juice with his warfarin. His INR hit 9.2 - normal is 2-3. He didn’t know the juice was the problem.
SSRIs and Grapefruit: Not All Are Equal
Not all SSRIs react the same way to grapefruit. It depends on which enzyme each one uses. Fluoxetine and paroxetine are mainly broken down by CYP2D6. Grapefruit has a weak effect on CYP2D6, so the risk here is low. But sertraline? That’s different. It’s metabolized by CYP2C9, CYP2C19, and CYP3A4 - the same enzyme grapefruit wrecks. A 2015 study found that people who drank grapefruit juice daily for two weeks saw their sertraline levels rise by 27-39%. That’s enough to cause dizziness, nausea, or even serotonin syndrome in rare cases.
Citalopram and escitalopram also use CYP3A4 and CYP2C19. But a March 2024 study in Clinical Pharmacology & Therapeutics found no significant interaction between escitalopram and grapefruit juice in healthy volunteers. That doesn’t mean it’s safe for everyone - just that the risk is lower than with sertraline. The American Psychiatric Association says grapefruit avoidance is only needed for sertraline in high-risk patients, like older adults or those on multiple meds.
Most people don’t realize this. A survey of medical students showed 64% thought all SSRIs had strong grapefruit interactions. Only 12% of SSRI users on Reddit mentioned grapefruit at all - and just 3% said they noticed side effects. But that doesn’t mean it’s not happening. Many symptoms - fatigue, brain fog, stomach upset - get blamed on the depression itself, not the juice.
Who’s at Highest Risk?
Not everyone needs to ditch grapefruit. But certain people are playing with fire:
- People on warfarin with CYP2C9 gene variants (genetic testing can confirm this)
- Those taking sertraline, especially if they’re older or on other meds
- Anyone taking multiple drugs metabolized by CYP3A4 (like statins, calcium blockers, or some anti-anxiety pills)
- Older adults, whose liver enzymes slow down naturally
Even healthy young people can be affected - but they’re less likely to notice because their bodies handle the extra drug load better. The real danger is in the silent buildup. No symptoms until it’s too late.
What Should You Do?
Here’s the practical advice - no guesswork:
- If you take warfarin, avoid grapefruit entirely unless you’ve had genetic testing showing you don’t have CYP2C9*2 or *3 variants.
- If you take sertraline, skip grapefruit. It’s not worth the risk. Other SSRIs like escitalopram or fluoxetine are safer bets.
- Check your other meds. Grapefruit interacts with over 85 drugs, including some statins, blood pressure pills, and anti-rejection drugs. Ask your pharmacist to run a quick check.
- Don’t assume orange juice is safe. Regular oranges are fine. But Seville oranges, pomelos, and tangelos? They’re grapefruit relatives - same problem.
- If you’ve been drinking grapefruit juice and just started a new med, watch for unusual side effects: dizziness, confusion, rapid heartbeat, or unexplained bruising.
Pharmacists at Mayo Clinic spend an average of 3.2 minutes per patient counseling on grapefruit interactions. That’s more time than they spend on most other food-drug issues. Why? Because it’s one of the few interactions that can’t be fixed by timing. You can’t outwait it. You have to avoid it.

The Bigger Picture
More than 1.2 million Americans take warfarin. Nearly 5 million take SSRIs. And 42% of U.S. adults take at least one drug that could interact with grapefruit. Yet only 18% of warfarin prescriptions and 8% of SSRI prescriptions include a grapefruit warning on the label. That’s a gap between science and practice.
The FDA is pushing for better labeling, especially after new data showed certain grapefruit varieties like Oroblanco and Sweetie have up to 300% more furanocoumarins than traditional ones. The European Medicines Agency predicts a 22% rise in grapefruit-related adverse events by 2030 if nothing changes.
For now, the rule is simple: if you’re on medication, ask your pharmacist or doctor - not Google - whether grapefruit is safe. And if you love the taste? Switch to oranges, apples, or berries. Your body will thank you.
Can I drink grapefruit juice if I take warfarin?
It’s safest to avoid it entirely. Grapefruit can interfere with CYP2C9 and CYP3A4 enzymes that break down warfarin, potentially raising your INR and increasing bleeding risk. Some people with certain gene variants (CYP2C9*2 or *3) are especially sensitive. Genetic testing can help determine your risk, but unless you’ve had that test, avoid grapefruit.
Do all SSRIs interact with grapefruit?
No. Only SSRIs metabolized by CYP3A4 or CYP2C9 are at risk. Sertraline is the main concern because it uses both. Citalopram and escitalopram have some risk, but recent studies suggest escitalopram is low-risk. Fluoxetine and paroxetine are mainly broken down by CYP2D6, which grapefruit affects only weakly - so they’re safer. Always check your specific medication.
How long does grapefruit affect CYP450 enzymes?
The effect lasts 24 to 72 hours after consumption. Grapefruit doesn’t just block the enzyme - it destroys it. Your body must grow new enzymes in your gut, which takes days. That’s why separating your juice and medication by a few hours doesn’t work. Avoid grapefruit entirely if you’re on a high-risk drug.
Is orange juice safe to drink with my meds?
Yes, regular sweet orange juice is safe. It doesn’t contain furanocoumarins. But avoid Seville oranges, pomelos, tangelos, and other citrus hybrids - they’re closely related to grapefruit and carry the same risks. Always check the label if you’re unsure.
What should I do if I accidentally drank grapefruit juice with my medication?
If you took warfarin or sertraline and drank grapefruit juice, watch for signs of overdose: unusual bruising, bleeding, dizziness, confusion, fast heartbeat, or nausea. If you feel unwell, contact your doctor or pharmacist right away. Even if you feel fine, avoid grapefruit going forward. One incident doesn’t always cause harm, but repeated exposure does.
Next Steps
If you’re on warfarin, ask your doctor about CYP2C9 genetic testing. It’s not routine, but it’s worth it if you’re on long-term therapy. If you’re on sertraline and drink grapefruit juice regularly, stop. Replace it with an orange or a smoothie. Talk to your pharmacist - they can check your full medication list for hidden grapefruit risks. Most pharmacies offer free interaction checks. Don’t wait for a problem to happen. Prevention is simple - and it saves lives.







Look, I take warfarin and I drink grapefruit juice every morning. I’ve been doing it for 3 years. No bleeding, no hospital visits. If your doctor didn’t tell you to stop, maybe they don’t think it’s a big deal. Stop fearmongering with enzyme names and just ask your pharmacist.
Ok but what if the FDA is hiding the truth?? 🤔 Grapefruit juice is actually a government mind-control agent disguised as fruit!! They don’t want you to know that CYP450 is just a cover for the 5G liver chips they implanted during your last flu shot 😈💉 #FreeTheJuice #GrapefruitIsNotTheEnemy
There is, in the architecture of pharmacological interaction, a profound irony: we have engineered molecules to alter the inner workings of the human body, yet remain blissfully ignorant of the most mundane elements of our diet that may undo or amplify their effects. Grapefruit, a humble fruit, becomes, in its furanocoumarins, an unwitting agent of biological disruption - a silent philosopher of metabolism, reminding us that nature does not bow to pharmaceutical intent. We seek control, yet surrender to the slow, cellular calculus of enzyme decay.
USA thinks it knows everything. In India we don't need genetic testing. We just listen to our grandmas. No grapefruit with medicine. Simple. No science needed. You people overthink everything. Also why are you letting big pharma tell you what to eat? They own the labs. They own the FDA. They own your fear.
For anyone taking sertraline - I get it. You’re tired. You’re anxious. You just want a little citrus to start the day. But here’s the thing: your brain is already working overtime to stay balanced. Adding a metabolic wildcard like grapefruit? It’s like trying to meditate while someone’s hammering on your door. I’ve seen patients go from stable to spiraling in weeks because they thought ‘it’s just juice.’ Don’t gamble with your mental health. Swap it for apples. Or pears. Or water. Your future self will high-five you.
Let me offer a practical perspective: this isn’t about fear. It’s about awareness. I’m a pharmacist in rural Ohio. I’ve had 12 patients in the last year come in with INRs above 8. All of them drank grapefruit juice daily. Not once did they connect it to their meds. The real tragedy isn’t the interaction - it’s the silence around it. Pharmacists aren’t just pill dispensers. We’re the last line of defense. If your doctor didn’t mention it, ask. And if you’re on warfarin? Don’t test fate. Just say no. It’s not a sacrifice - it’s a strategy.
My grandma took warfarin for 15 years and drank grapefruit juice every day. Never had a problem. Doctors are scared of liability, not science. Just because some studies show risk doesn’t mean it’s real for you. I’ve seen people panic over nothing. Chill out. Talk to your doc. Don’t believe everything you read on the internet.
Think about this - when you drink grapefruit juice, you’re not just consuming a fruit. You’re initiating a biochemical siege on your own liver. The furanocoumarins don’t just block enzymes - they annihilate them. Like setting fire to a library of instruction manuals your body uses to decode every pill you swallow. And here’s the kicker: your body doesn’t just rebuild those manuals. It has to relearn how to read them from scratch. That’s why timing doesn’t matter. That’s why one glass ruins your whole week. That’s why your doctor’s advice isn’t just a suggestion - it’s a survival protocol. And yet, we treat it like a dietary preference. We’re not just careless. We’re culturally negligent.
Just to clarify: the 2024 Clinical Pharmacology & Therapeutics study on escitalopram was a randomized, double-blind, placebo-controlled trial with 48 healthy volunteers - not observational data. The lack of interaction was statistically significant (p < 0.01). That’s not a minor finding. It’s a clinically meaningful distinction. Please stop lumping all SSRIs together. Precision matters. Especially when lives are on the line.
So we’re supposed to fear a fruit because some lab rats got high on serotonin? What’s next? Ban sunlight because it might mess with your vitamin D levels? This is what happens when you let PhDs with Excel sheets decide what you can eat. I’ll take my grapefruit and my sertraline and my freedom thanks
STOP.