Every year, thousands of patients in the UK and US receive the wrong medication-not because of a doctor’s mistake, but because two bottles looked too similar. A pill labeled hydralazine sits next to one labeled hydroxyzine. Two insulin pens, nearly identical in size and colour, sit side by side in the fridge. A pharmacist grabs the wrong one during a busy shift. The result? A patient gets a drug meant for high blood pressure instead of allergies-or worse. These aren’t hypotheticals. They’re real, preventable errors that happen in pharmacies every day.
Why Look-Alike Packaging Is a Silent Killer
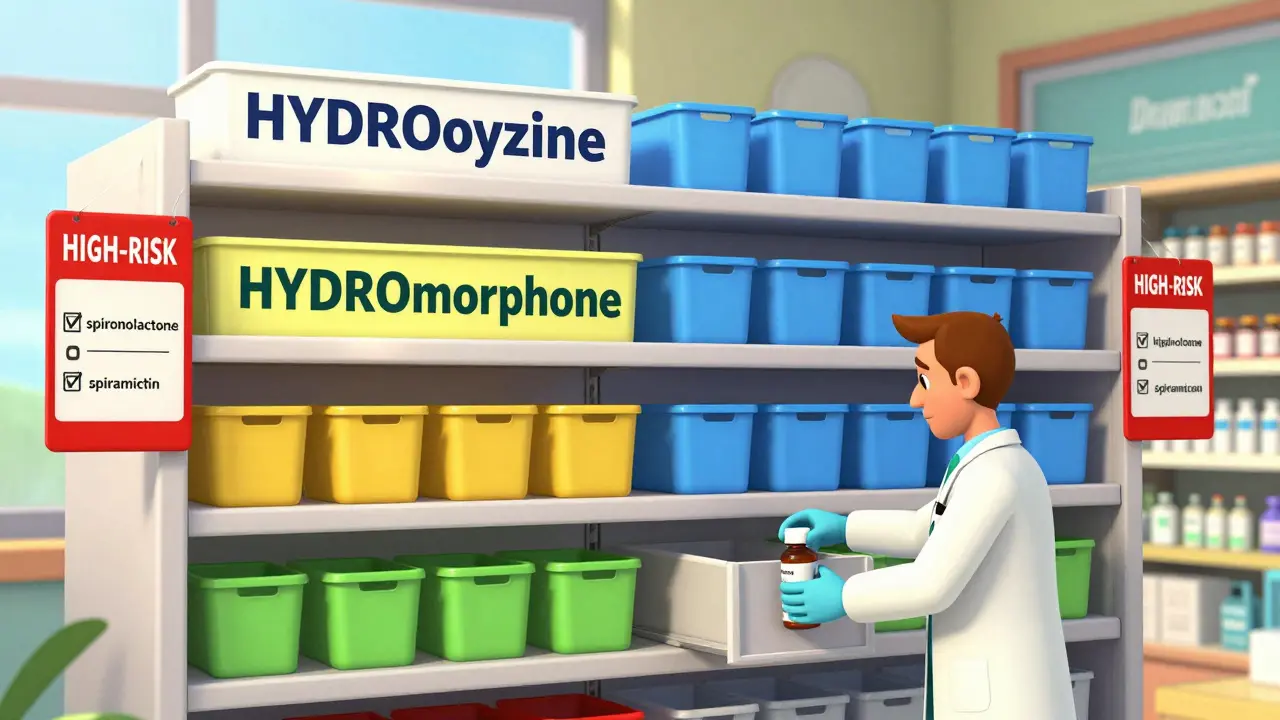
The problem isn’t new. Since the 1970s, pharmacists have been warning about drugs that look or sound alike. But it’s only in the last decade that the scale became clear. According to the Institute for Safe Medication Practices (ISMP), about 18% of all medication error reports in the US are tied to look-alike or sound-alike (LASA) drugs. That’s roughly 10,000 reported incidents annually. The real number? Likely much higher. Many errors go unreported-especially in community pharmacies where staff are stretched thin. The danger isn’t just in the names. Packaging plays a huge role. Two drugs might have very different names, but if their bottles, caps, labels, and fonts are nearly identical, the brain doesn’t notice the difference. A 2020 study from the University of Arizona found that simply separating look-alike drugs in storage cut errors by 62%. That’s not a small win-it’s life-saving.Physical Separation: The Simplest Fix
You don’t need fancy tech to start reducing errors. The most effective first step? Move similar-looking drugs apart. In hospital pharmacies, this means using dedicated drawers in automated dispensing cabinets (ADCs). One drawer for all insulin types. Another for all anticoagulants. No mixing. No guesswork. In community pharmacies, where space is tight, shelf dividers cost less than £500 and can make a huge difference. Place high-risk pairs like spironolactone and spiramycin on opposite ends of the shelf. Use colour-coded bins or sticky labels to flag them. One pharmacy in Manchester reported a 75% drop in wrong-drug dispensing after they started using red alert labels on LASA pairs. The key? Consistency. If you separate them today but let them get mixed again next week, the risk returns. Make physical separation part of your daily workflow. Train new staff on it. Include it in your checklist.Tall Man Lettering: Making Names Harder to Mix Up
Sometimes, the drugs aren’t just similar in packaging-they’re similar in name. That’s where Tall Man Lettering (TML) comes in. TML uses capital letters to highlight the differences between similar drug names:- DOPamine vs. DoBUTamine
- HYDROmorphone vs. HYDROxyzine
- BUPREnorphine vs. BUTORphanol

Barcode Scanning: The Safety Net
Physical separation and TML are great-but they’re not foolproof. People still make mistakes. That’s where barcode scanning becomes essential. When a pharmacist scans the drug and the patient’s wristband before dispensing, the system checks: Is this the right drug? Right dose? Right patient? If there’s a mismatch, it alarms. A 2021 AHRQ report found this reduces medication administration errors by 86%. The downside? Cost. Full implementation can run £15,000-£50,000 per pharmacy. But the savings are even bigger. Mayo Clinic’s program saved £220,000 a year by preventing errors-far more than the £30,000 it cost to set up. Even if you can’t afford full automation, start small. Use barcode scanners for high-risk drugs first-insulin, heparin, opioids. Train staff not to bypass the scan. One study found 5-12% of scans were skipped during peak hours. That’s when errors spike.Combining Strategies: The 94% Solution
The best results come from stacking methods. A 2023 study in the American Journal of Health-System Pharmacy found that pharmacies using all three strategies-physical separation, Tall Man Lettering, and barcode scanning-cut errors by 94%. Think of it like seatbelts, airbags, and ABS in a car. One helps. All three save lives. Start with physical separation. It’s cheap and fast. Then add TML to your system. Finally, invest in barcode scanning for your highest-risk medications. Don’t wait for perfection. Start with one step. Then add the next.What to Do When New Drugs Arrive
New medications hit the shelves every week. Some are designed to look like existing ones-intentionally or not. That’s why every new drug should trigger a quick review. When a new product arrives, ask:- Does it look like any drug we already stock?
- Does its name sound like another?
- Is it on ISMP’s updated List of Confused Drug Names (2024)?

Common Pitfalls and How to Avoid Them
Not all solutions work everywhere. Here’s what goes wrong-and how to fix it:- "We don’t have space." Use vertical dividers, labelled bins, or even coloured tape on shelves. You don’t need a new layout-just better organisation.
- "Staff forget to scan." Make scanning mandatory. Tie it to your quality checks. If someone skips it, it’s flagged in your audit.
- "Our software doesn’t support TML." Talk to your vendor. Most EHR systems can be updated. If they won’t help, push back. Patient safety isn’t optional.
- "It’s not my problem." Everyone in the pharmacy has a role. Technicians, pharmacists, even receptionists who hand out prescriptions. Train them all.
The Future Is Already Here
The next wave of LASA prevention is smarter technology. Pilot programs at Johns Hopkins are testing AI systems that scan drug packaging images and flag visual similarities before a drug even reaches the shelf. These systems can spot mismatches in font size, colour contrast, or label layout-things humans miss. The National Council for Prescription Drug Programs (NCPDP) is also working on a standard LASA data format, due to launch in late 2025. This will let systems automatically flag risky pairs across pharmacies, hospitals, and prescriptions. This isn’t science fiction. It’s coming fast. The question isn’t whether you’ll need it-it’s whether you’ll be ready.Start Today. Save Lives Tomorrow.
You don’t need a big budget to make a big difference. Start with one thing:- Identify your top 5 most dangerous look-alike pairs.
- Separate them physically this week.
- Add Tall Man Lettering to your system by next month.
- Train your team to scan before dispensing.
What are the most common look-alike drug pairs in UK pharmacies?
The most frequent pairs include hydralazine and hydroxyzine, spironolactone and spiramycin, insulin glargine and insulin lispro, and heparin and saline. ISMP’s 2024 update added buprenorphine and butorphanol as high-risk pairs. Always check their latest list quarterly.
Can Tall Man Lettering prevent all packaging errors?
No. Tall Man Lettering only helps with name confusion. About 35% of LASA errors come from packaging similarities-similar bottle shapes, cap colours, or label layouts. That’s why you need physical separation and barcode scanning too.
Is barcode scanning worth the cost for small community pharmacies?
Yes, if you handle high-risk drugs like insulin, opioids, or anticoagulants. The cost can be offset by preventing just one serious error. Start with a single scanner for those top 5 high-risk medications. Many vendors offer affordable, modular systems.
How often should I review my pharmacy’s LASA risks?
At least every quarter, when ISMP releases its updated list. Also review after any new drug arrives, after a near-miss incident, or if you’ve had a dispensing error. Don’t wait for something bad to happen.
What’s the easiest way to get staff to follow new safety steps?
Make it part of your daily checklist and tie it to your quality audits. If scanning or separation is checked off during routine reviews, compliance improves. Also, share success stories-like how your error rate dropped after implementing separation. People respond to results, not rules.






man i just saw a bottle of hydralazine next to hydroxyzine at my local chemist last week-looked like twins. no wonder people get messed up. they dont even label em right. my aunt got the wrong one n ended up in A&E. total chaos.
It is, frankly, an egregious oversight that healthcare institutions continue to permit such egregious visual homologues in pharmaceutical packaging. The Institute for Safe Medication Practices has published unequivocal guidelines since 2007-yet compliance remains abysmal. This is not merely negligence; it is a systemic failure of institutional responsibility.
I’ve worked in three different hospitals across the U.S., and I can tell you-physical separation works. We started putting all insulin pens in one locked drawer with a bright yellow label. Errors dropped by 70% in six months. No fancy tech. Just common sense. It’s heartbreaking that so many pharmacies still ignore this.
bro u gotta use tall man lettering like HYDROxyzine vs HYDROmorphone-so simple but so effective. my pharmacy in mumbai started using it last year and we had zero mixups since. also, get ur EHR to auto-format it. dont rely on staff to type it right. tech should help, not hurt.
Let’s be honest-barcodes are overrated. Most errors happen before the scan, during selection. If your shelves are a mess, no scanner in the world will save you. Focus on layout first. Then tech. Always.
Thank you for writing this with such care and clarity. As someone who’s lost a loved one to a medication error, I can’t tell you how much this means. The fact that simple, low-cost solutions like colored bins and Tall Man Lettering can prevent so much suffering-it’s almost too easy not to act. Please keep sharing this. We need more voices like yours.
Y’all are overcomplicating this. Put the scary drugs on the top shelf. Put the rest on the bottom. Done. No scanners, no software, no meetings. Just move the damn bottles. I’ve done it in 3 pharmacies. Saved lives. Simple as that.
Why are we even talking about this? In the U.S., we’ve got real problems-like illegal drugs flooding the streets. This is just bureaucratic overreach disguised as safety. If people can’t read labels, maybe they shouldn’t be taking pills.
Barcode scanners? Waste of cash. We don’t need them. Just train people. Simple.
My cousin works in a small pharmacy in Delhi. They use sticky notes with big red 'DANGER' on similar bottles. No tech. No budget. But they never made a mistake. Start small. Do something. Anything.