When your liver is damaged, blood doesn’t flow the way it should. Instead of moving smoothly through the organ, it backs up-like water trapped behind a clogged pipe. This backup creates portal hypertension, a serious condition that doesn’t cause symptoms on its own but sets the stage for deadly complications: bleeding varices, fluid-filled abdomen (ascites), and brain fog from hepatic encephalopathy. If you or someone you know has cirrhosis, understanding how these complications develop and how to stop them isn’t just helpful-it’s life-saving.
What Exactly Is Portal Hypertension?
Portal hypertension isn’t a disease by itself. It’s a consequence. The portal vein carries blood from your intestines, spleen, and pancreas to your liver. When the liver is scarred-usually from years of alcohol abuse, hepatitis, or fatty liver disease-this blood can’t flow through easily. The pressure in the vein rises. The medical definition? A hepatic venous pressure gradient (HVPG) of more than 5 mmHg. Clinically significant portal hypertension starts at 10 mmHg. That’s the tipping point where things start going wrong.About 90% of cases come from cirrhosis. The other 10%? Non-cirrhotic causes like blood clots in the portal vein, rare infections, or genetic conditions. But cirrhosis is the big one. And here’s the scary part: within five years of being diagnosed with cirrhosis, about 70% of people will develop portal hypertension. It’s not rare. It’s predictable. And it’s dangerous.
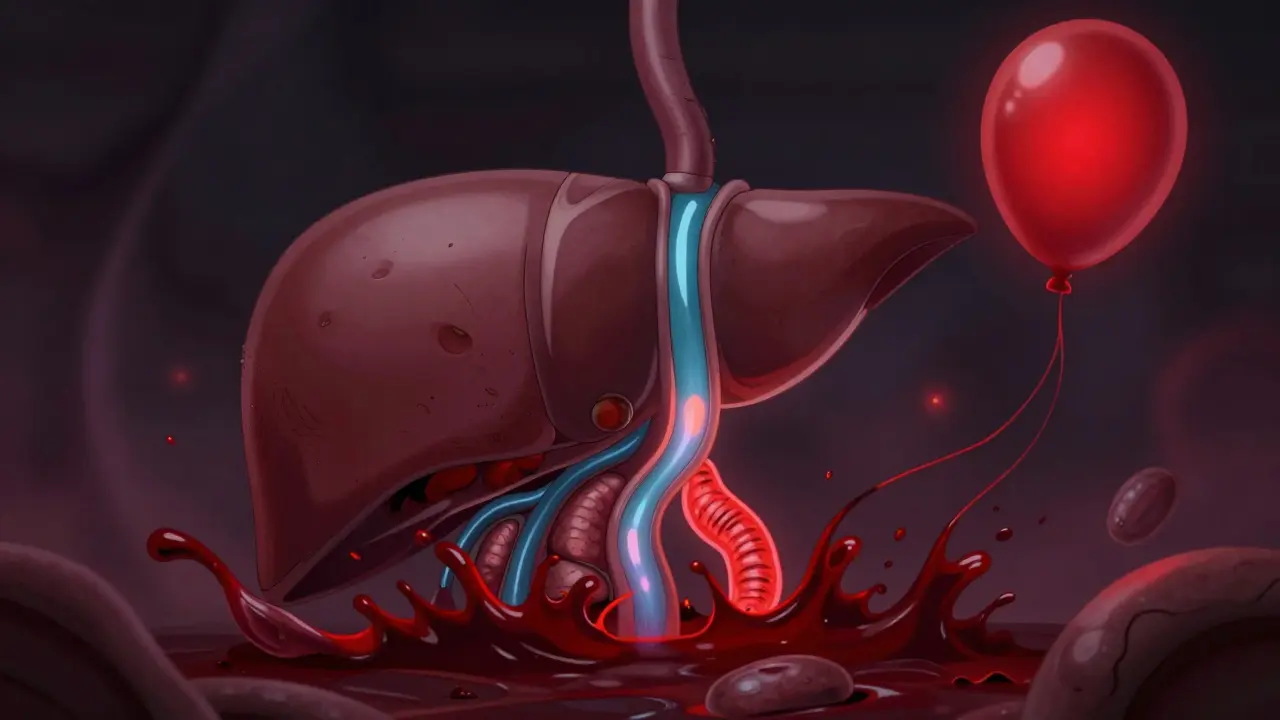
Varices: The Silent Time Bomb
As pressure builds, blood looks for new paths. It finds them-in the veins of your esophagus and stomach. These veins aren’t built to handle high pressure. They swell, stretch, and thin out. These are varices. Think of them like bulging garden hoses. One small tear, and you’re bleeding internally.Half of all people with cirrhosis develop varices within ten years. And once they’re there, the risk of bleeding is real: 5% to 15% per year. A bleed isn’t just a medical emergency-it’s terrifying. People describe vomiting bright red blood, black tarry stools, dizziness, passing out. About 15% to 20% of people who bleed die within six weeks. That’s the grim reality.
But it doesn’t have to be this way. Screening with endoscopy is standard for anyone with cirrhosis. If medium or large varices are found, treatment starts immediately. The gold standard? Endoscopic band ligation. A tiny rubber band is placed around the varix, cutting off its blood supply. It’s quick, minimally invasive, and reduces rebleeding from 60% down to 20-30%. Beta-blockers like propranolol also help. They lower heart rate and blood pressure in the portal system. Studies show they cut the first bleeding risk by nearly half. The goal? Reduce HVPG to below 12 mmHg or by at least 20% from baseline. That’s the target doctors aim for.
Ascites: When Fluid Fills Your Belly
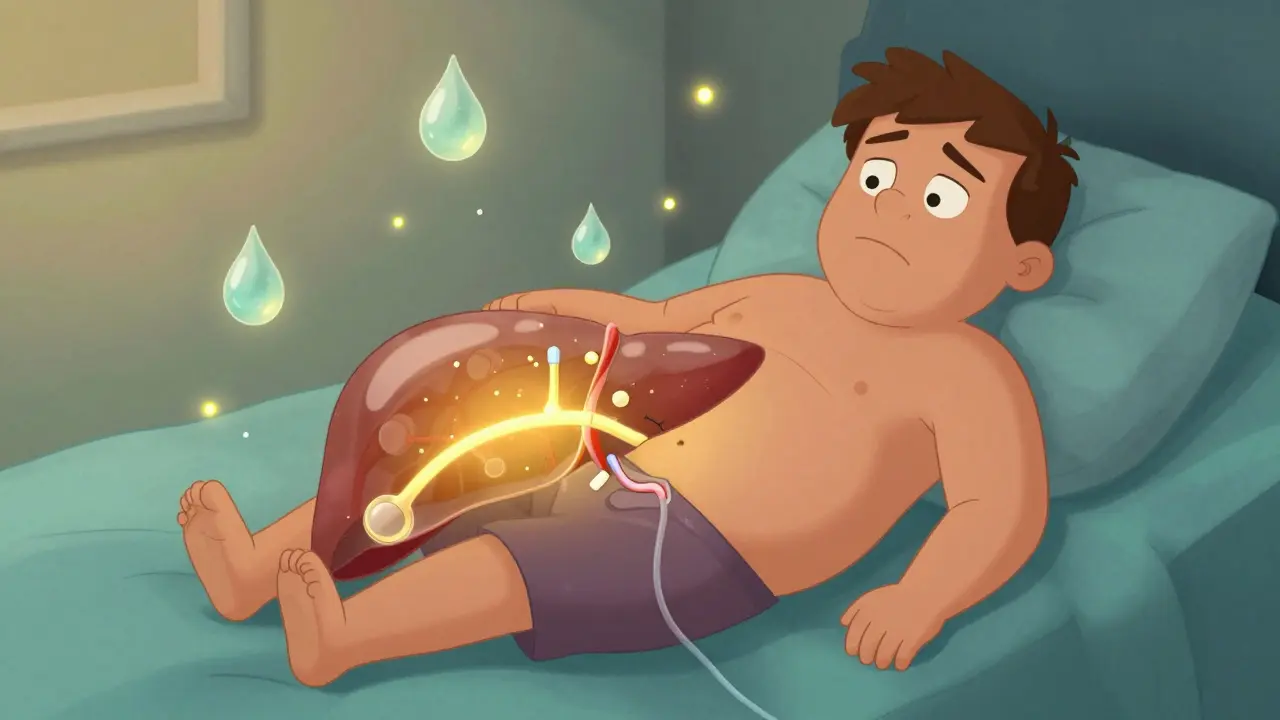
Another consequence of portal hypertension? Fluid leaks out of blood vessels into your abdomen. This is ascites. It affects 60% of cirrhotic patients within ten years. At first, it’s just a feeling of fullness. Then your belly swells. You get short of breath. You can’t tie your shoes. Some people gain 20 pounds of fluid in weeks.Management starts simple: salt restriction. Less than 2,000 mg per day. Then diuretics-spironolactone and furosemide. These help your kidneys flush out extra fluid. For most, this works. But when it doesn’t? That’s called refractory ascites. You need a procedure called paracentesis: a needle inserted into your belly to drain liters of fluid. It gives immediate relief, but the fluid comes back. And every time you drain more than 5 liters, you need albumin-human protein-infused to prevent dangerous drops in blood pressure.
For those with recurring ascites, TIPS (transjugular intrahepatic portosystemic shunt) is an option. A stent is placed inside the liver to create a shortcut between the high-pressure portal vein and the low-pressure hepatic vein. It works in 90-95% of cases. But there’s a catch: up to 30% of people develop hepatic encephalopathy afterward. Confusion, forgetfulness, even coma. So TIPS isn’t for everyone. It’s a trade-off: better fluid control versus brain function risk.
Other Complications You Can’t Ignore
Portal hypertension doesn’t stop at bleeding and fluid. It triggers a chain reaction.Hepatic encephalopathy affects up to 45% of cirrhotic patients. Toxins your liver can’t filter build up in your blood and reach your brain. You might feel sluggish, forget names, have trouble concentrating. In severe cases, you slip into a coma. Lactulose and rifaximin are the main treatments. They clean out gut bacteria that produce these toxins.
Hepatorenal syndrome is another silent killer. Your kidneys start failing-not because they’re damaged, but because your body’s circulation is so messed up from portal hypertension. It happens in 18% of hospitalized cirrhotic patients with ascites. Survival without a transplant is grim. Often, it’s a sign that liver transplant is the only real solution.
And then there’s the emotional toll. Patients on forums talk about quitting jobs because they can’t stand for more than 20 minutes. They live in fear of the next bleed. One Reddit user wrote: “I spent three days in the ICU after vomiting liters of blood. Now I live with the constant fear it’ll happen again.” This isn’t just physical-it’s psychological. Quality of life scores for these patients are 35-40 points lower than healthy peers.
What’s New in Treatment?
The field is changing fast. For years, we focused only on lowering pressure. Now, we’re looking at the whole picture. Experts like Dr. Patrick Northup say we need to consider cardiac output and systemic resistance-not just the liver.Non-invasive tools are getting better. Spleen stiffness measurement via elastography now predicts clinically significant portal hypertension with 85% accuracy. That could mean fewer invasive HVPG tests. In September 2023, the European Medicines Agency approved the Hepatica SmartBand-a wearable device that estimates portal pressure using bioimpedance. It’s not perfect (82% accurate), but it’s a step toward continuous monitoring.
Drug development is also moving forward. Simtuzumab, a monoclonal antibody targeting liver scarring, got FDA breakthrough designation in October 2023. Early trials showed a 35% drop in HVPG. Twelve new drugs are now in phase 2 trials aiming to reduce pressure without causing dangerous drops in blood pressure elsewhere.
AI is helping too. Mayo Clinic’s algorithm predicts variceal bleeding with 92% accuracy by analyzing imaging, lab values, and clinical history. That means we can start preventive treatment before the first bleed happens.
When Is a Transplant the Only Option?
For some, no matter how well you manage varices and ascites, the liver keeps failing. That’s when transplant becomes the only long-term answer. But waiting lists are long. In the U.S., the average wait is 14 months. And not everyone qualifies. You need to be sober (if alcohol-related), free of active infection, and mentally prepared. Still, for those who make it, survival rates are high-over 80% at five years.But transplant isn’t a cure-all. Portal hypertension can return if the new liver gets diseased again. That’s why managing the underlying cause-whether it’s stopping alcohol, controlling hepatitis, or losing weight for fatty liver-is just as important after transplant as before.
What You Can Do Right Now
If you have cirrhosis or know someone who does:- Get screened for varices with an endoscopy. Don’t wait for symptoms.
- If you’re on beta-blockers, don’t stop them without talking to your doctor. They save lives.
- Track your salt intake. Read labels. Avoid processed food.
- Know the signs of bleeding: black stools, vomiting red blood, dizziness.
- Ask about HVPG testing. It’s not available everywhere, but it’s the best way to measure severity.
- Consider non-invasive tests like FibroScan or ELF if your clinic offers them.
Portal hypertension won’t go away. But its worst consequences can be prevented. The key is early detection, consistent treatment, and never ignoring the warning signs. This isn’t about hoping for the best. It’s about planning for the worst-and stopping it before it starts.






Been living with cirrhosis for 7 years. Varices got me once-vomited blood in the grocery store parking lot. Scary as hell. Band ligation saved my life. Beta-blockers? Non-negotiable. Salt? I weigh mine now. It’s not glamorous, but it’s how you stay alive.
Also, that Hepatica SmartBand thing? I’d wear it if it meant not having to go in for another HVPG. No thanks to needles.
It is imperative to underscore that portal hypertension is not an incidental finding, but rather a pathophysiological inevitability in the context of advanced hepatic fibrosis. The notion that non-invasive modalities such as spleen elastography may supplant hemodynamic assessment is, frankly, premature. The HVPG remains the gold standard for a reason: it quantifies the pressure gradient directly, not inferentially. To rely on bioimpedance or AI algorithms without histological correlation is to engage in medical speculation masquerading as innovation.
Bro. I just read this whole thing and I’m like… 🤯
So like, if you got cirrhosis, you’re basically playing Jenga with your organs and the liver is the bottom block? One wrong move (like drinking, or eating a bag of chips) and WHAM-bleeding, brain fog, belly full of water.
Also-Hepatica SmartBand?? That’s a real thing?? I’m ordering one. 😎🩺
In India, many patients never get screened. No access. No money. No awareness. I’ve seen men in rural clinics with ascites so severe they can’t lie flat-and they’re told to ‘eat less salt’ and sent home. The gap between what’s written here and what’s practiced is a canyon.
Transplant? Only in metros. And even then, it’s a lottery. We need public health systems that treat this like the emergency it is.
OKAY. I NEED TO SAY THIS.
THEY PUT A RUBBER BAND INSIDE YOUR ESOPHAGUS.
LIKE A TINY, BLOOD-FILLED BALLOON THAT JUST… SNAPS.
AND YOU’RE ALIVE TO TELL THE STORY.
THIS IS NOT MEDICINE. THIS IS A SUPERHERO MOVIE.
AND SOMEONE JUST TOLD YOU TO ‘WATCH YOUR SALT’ LIKE IT’S A DIET PLAN.
WE ARE LIVING IN A NIGHTMARE THAT’S BEEN CLINICALLY DOCUMENTED.
WHY ISN’T THIS ON THE NEWS?
WHY ISN’T THERE A MOVIE?
WHY ISN’T EVERYONE SCARED?
…I’m crying. I’m not okay.
But I’m also gonna get my endoscopy. Tomorrow.
I’m a nurse and I see this every week. One guy came in with black stools and just said ‘I thought it was from the iron pills.’
He didn’t know he had cirrhosis until he almost died.
Y’all. Please. Get checked. Even if you think you’re fine. It’s silent until it’s not.
And if you’re on beta-blockers? Don’t skip them. I’ve seen too many come back.
Love you all. Stay safe.
What if portal hypertension isn’t a disease at all… but a whisper from the body saying: you’ve been living in opposition to your own nature?
The liver doesn’t hate you. It’s just exhausted.
Alcohol. Sugar. Stress. Silence.
It’s been carrying your chaos for decades.
And now it’s asking for peace.
Maybe the real cure isn’t a band. Or a shunt.
Maybe it’s learning to stop drowning yourself.
And just… breathe.
…I’m not a doctor. But I’ve watched my mother die from this.
And she never stopped drinking.
So I guess… I’m just asking: are we treating the body… or just the symptom?
Does anyone know if the AI algorithm from Mayo Clinic is available to the public? Or is it only for hospitals? I’m asking because my dad has cirrhosis and we’re trying to figure out how to get him screened properly. We don’t live near a big medical center.
Also-has anyone tried FibroScan? Is it worth asking for?