Dermatomyositis: Quick Guide to Symptoms, Tests, and Treatment
Dermatomyositis is an autoimmune condition that causes a telltale skin rash and muscle weakness. If you’ve noticed unusual purple or red patches on your eyelids, knuckles, or chest plus trouble climbing stairs or lifting things, don’t ignore it. Early recognition changes outcomes — treatments work better when started sooner.
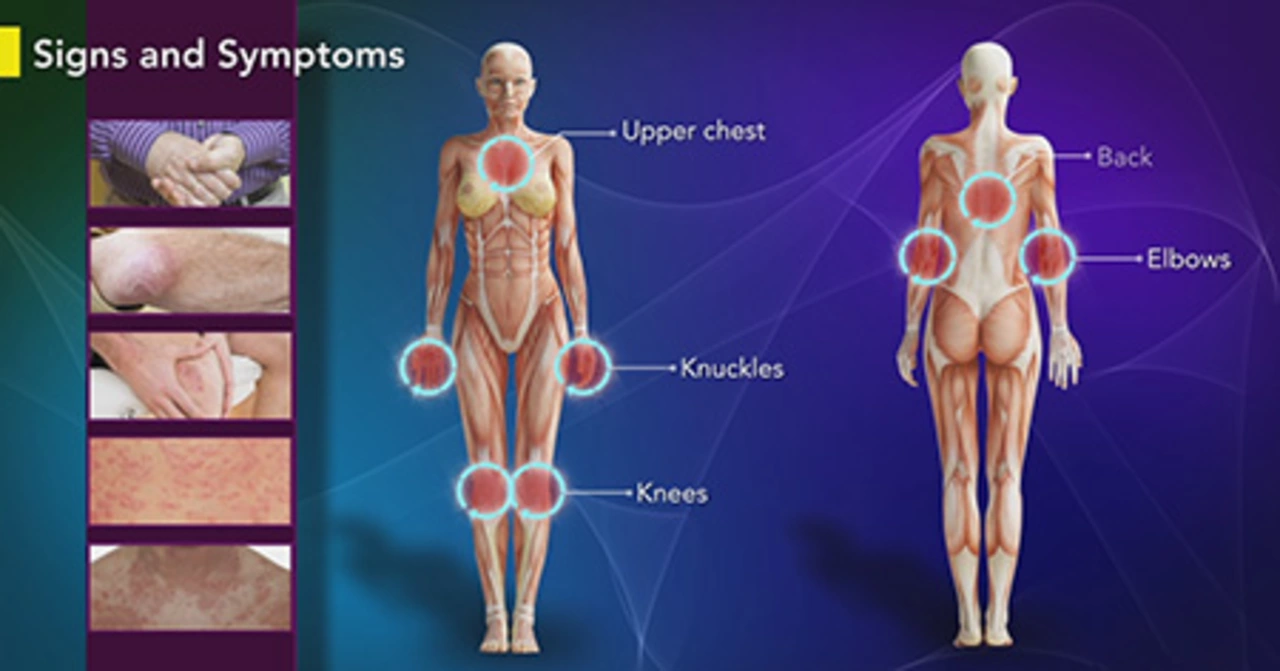
Spot the signs early
Common clues include a heliotrope rash (purple around the eyes), Gottron’s papules (scaly bumps over knuckles), and progressive muscle weakness in the hips and shoulders. Fatigue and difficulty swallowing can show up too. Some people get joint pain, lung symptoms (shortness of breath), or unexplained fevers. Because dermatomyositis can affect other organs, any new breathing trouble or trouble swallowing should prompt urgent evaluation.
Doctors usually check blood tests first: creatine kinase (CK) or aldolase often rise with muscle damage. Autoantibody panels can point to specific subtypes. Imaging like MRI helps find inflammation in muscles, while electromyography (EMG) looks at electrical activity. A muscle biopsy gives the clearest diagnosis when tests are unclear.
Treatment options and real-world tips
Start with medicines that reduce immune attack. High-dose corticosteroids (prednisone) are the usual first step to bring inflammation down quickly. Because long-term steroid use has side effects, steroid-sparing drugs are commonly added: methotrexate, azathioprine, or mycophenolate. Recent options include JAK inhibitors for people who don’t respond to older meds.
If skin symptoms are severe, topical steroids or antimalarials like hydroxychloroquine can help. For lung involvement, your doctor may choose stronger immunosuppression and more frequent monitoring of lung function. Physical therapy is key: gentle, supervised exercise preserves strength and mobility without worsening inflammation.
Watch for complications: interstitial lung disease and increased cancer risk in some adults. Your care team should include a rheumatologist or neurologist, and may add a dermatologist, pulmonologist, or oncologist depending on symptoms. Regular screening and age-appropriate cancer checks are often recommended.
Practical steps to take now: write down symptoms and when they started, bring photos of rashes that come and go, ask your doctor for CK and antibody tests, and request a referral to a specialist if symptoms are getting worse. Ask about steroid side effects and the plan to taper or add steroid-sparing drugs.
Manage daily life with sun protection (rashes flare with UV exposure), balanced nutrition, and pacing activities to avoid crashes. For medication questions — interactions, monitoring, or options if you can’t tolerate one drug — have a short list of concerns for your visit so you get clear answers.
If you need more in-depth guides on specific drugs, monitoring, or safely sourcing medications online, look for trusted clinic resources or talk directly with your pharmacy team. Dermatomyositis can be managed — but it takes a team and a clear, practical plan.