Laryngopharyngeal Reflux (LPR): Quick, Practical Help for Throat Reflux
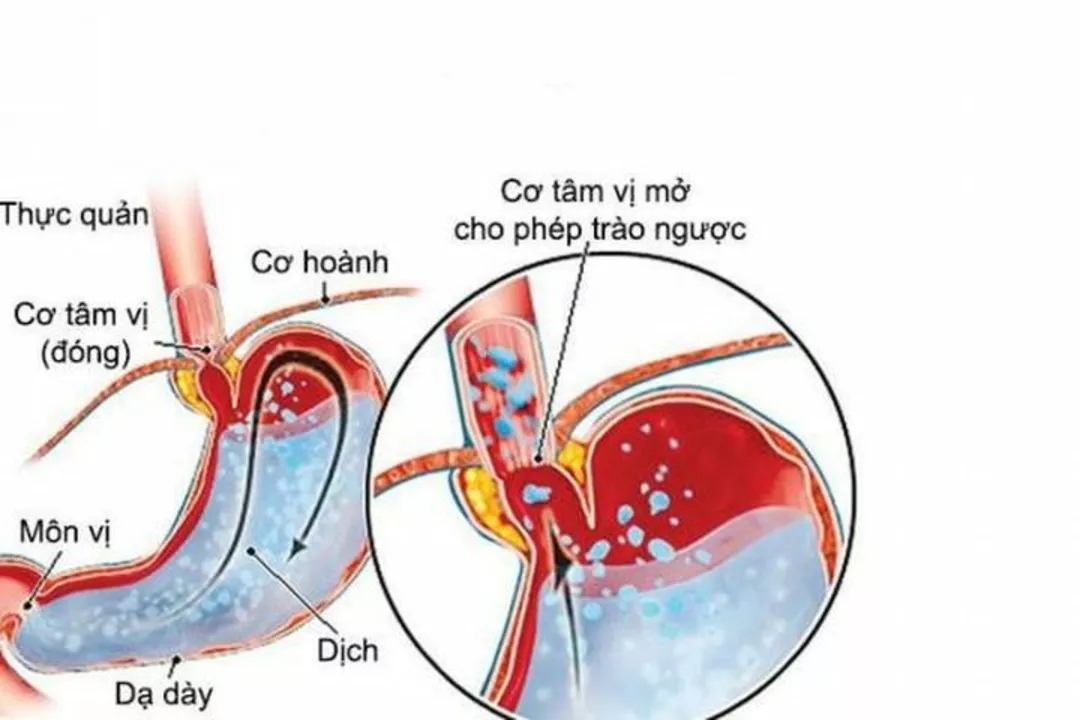
Do you often clear your throat, sound hoarse, or feel a lump in your throat without the classic heartburn? That could be laryngopharyngeal reflux (LPR), sometimes called "silent reflux." It sends stomach acid or enzymes up high enough to irritate the throat and voice box.
LPR is not the same as typical GERD. With GERD you usually get heartburn and acid taste. With LPR the main problems are throat-related: chronic cough, throat clearing, hoarseness, a constant lump sensation (globus), postnasal drip, or a sore throat that won’t quit. Nighttime coughing and feeling that food sticks can also appear.
How doctors check for LPR
An ENT (ear, nose and throat) doctor will often start with a simple exam and a laryngoscopy — a quick look at your vocal cords using a flexible camera. Redness, swelling, or mucus on the larynx raises suspicion. To confirm reflux, tests like 24-hour pH monitoring or impedance testing can measure acid and non-acid reflux. Sometimes doctors use a short trial of medication to see if symptoms improve — that can be both diagnostic and therapeutic.
Other issues can mimic LPR (allergy, asthma, postnasal drip, vocal strain), so expect a careful look at your voice use, allergies, and medications that might loosen the lower esophageal sphincter.
Simple steps you can try today
Start with practical changes that often help. Eat smaller meals and avoid late dinners — stop eating at least 2–3 hours before lying down. Raise the head of your bed 6–8 inches or use a wedge; this keeps stomach contents lower while you sleep. Quit smoking and cut alcohol and caffeine — they relax the valve that keeps acid down.
Watch common food triggers: spicy foods, fatty or fried meals, chocolate, peppermint, citrus, tomatoes, and carbonated drinks. Try chewing sugar-free gum after meals to boost saliva and clear acid. If you clear your throat a lot, work with a speech therapist; simple voice therapy reduces throat clearing and gives your irritated tissues a chance to heal.
Medications often used include proton pump inhibitors (PPIs), H2 blockers, and alginate preparations that form a protective raft. PPIs are commonly prescribed for several weeks; discuss risks and benefits with your doctor before starting. In stubborn cases, surgery or endoscopic options may be considered, but that’s uncommon.
When to see a doctor? If symptoms last more than 6–8 weeks despite simple measures, cause weight loss, difficulty swallowing, or blood in saliva, get evaluated. Also see a specialist if voice changes affect work or singing.
Want to learn more? Read related guides on diet, digestive health, and safe medication use on BuyBestMeds.com. If you’re unsure about tests or treatment, book a visit with an ENT or your primary care clinician — clear answers usually start with a focused exam and a few practical steps.
Related reads: "Effective Ways to Prevent Acute Diarrhea and Boost Digestive Wellness" — gut health basics; "Ginger Benefits" — what ginger can and can’t do; "Natural Solutions: Magnesium Hydroxide for Constipation Relief" — gentle options for digestion; "Pregnancy and Decongestants" — special considerations if you’re pregnant and dealing with throat symptoms.