Pituitary gland: the small master that controls your hormones
The pituitary gland is about the size of a pea, but it runs big parts of your body—growth, stress response, thyroid function, reproduction, even water balance. When it works well you barely notice it. When it doesn’t, symptoms can be subtle or sudden and confusing. This page gives clear, practical info on what the pituitary does, common problems, how doctors check it, and next steps you can take.
How the pituitary works and why it matters
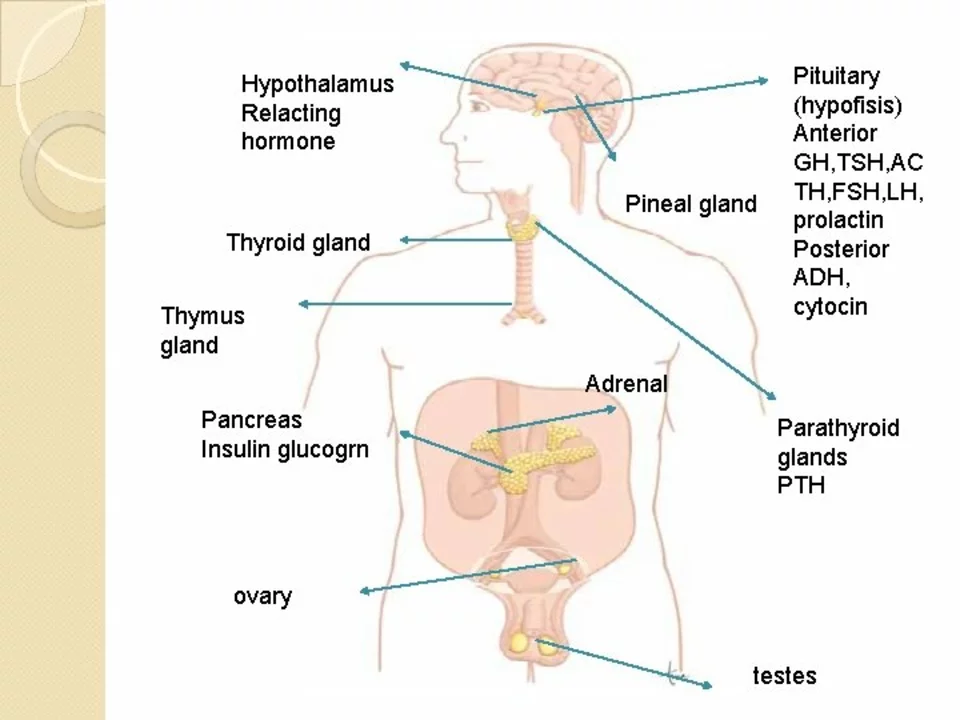
The pituitary sits under the brain and secretes hormones that tell other glands what to do. Think of it as a control hub: it prompts the thyroid, adrenals, ovaries or testes, and controls growth and water balance. A tiny tumor (almost always benign) or injury can change hormone levels up or down. That shift can cause fatigue, weight changes, irregular periods, low libido, headaches, vision problems, or unexplained muscle weakness.
Common problems, tests, and treatment options
Common pituitary issues include pituitary adenomas (hormone-secreting or not), hypopituitarism (low pituitary output), prolactinomas, Cushing’s disease, and acromegaly. To check the gland, doctors usually order blood tests for hormone levels—TSH, ACTH, cortisol, prolactin, LH, FSH, IGF-1—and an MRI of the pituitary. If vision is affected, an eye exam is part of the workup.
Treatment depends on the problem. Small, non-secreting tumors may just be watched with regular MRIs and blood tests. Prolactinomas often respond to dopamine agonist pills (cabergoline or bromocriptine). Acromegaly and some hormone-secreting tumors may need surgery, medication (somatostatin analogs, GH receptor blockers), or targeted radiation. If the pituitary is underactive, hormone replacement (thyroid hormone, cortisol, sex hormones) is the main option. Your endocrinologist will tailor the plan to your needs.
Emergency signs—severe headache, sudden vision loss, fainting, very low blood pressure—need urgent care. That can signal pituitary apoplexy (bleeding into the gland) which requires immediate treatment.
Want practical steps now? Keep a symptom diary (sleep, weight, mood, menstrual changes, thirst), bring it to your GP, and ask for basic hormone tests and an MRI referral if symptoms point to the pituitary. A referral to an endocrinologist is common and helpful.
On this site we cover related topics that can help you understand tests, medicines, and side effects. Check articles like “Prednisone Alternatives for Autoimmune Diseases: Azathioprine, Mycophenolate, and JAK Inhibitors” for steroid context, “Accutane: The Real Story About Isotretinoin” for hormone-linked skin treatment notes, and our pharmacy reviews if you need reliable medication sources.
If something feels off, don’t brush it off. Small gland, big effects—get a proper check so you can get the right treatment and feel better sooner.