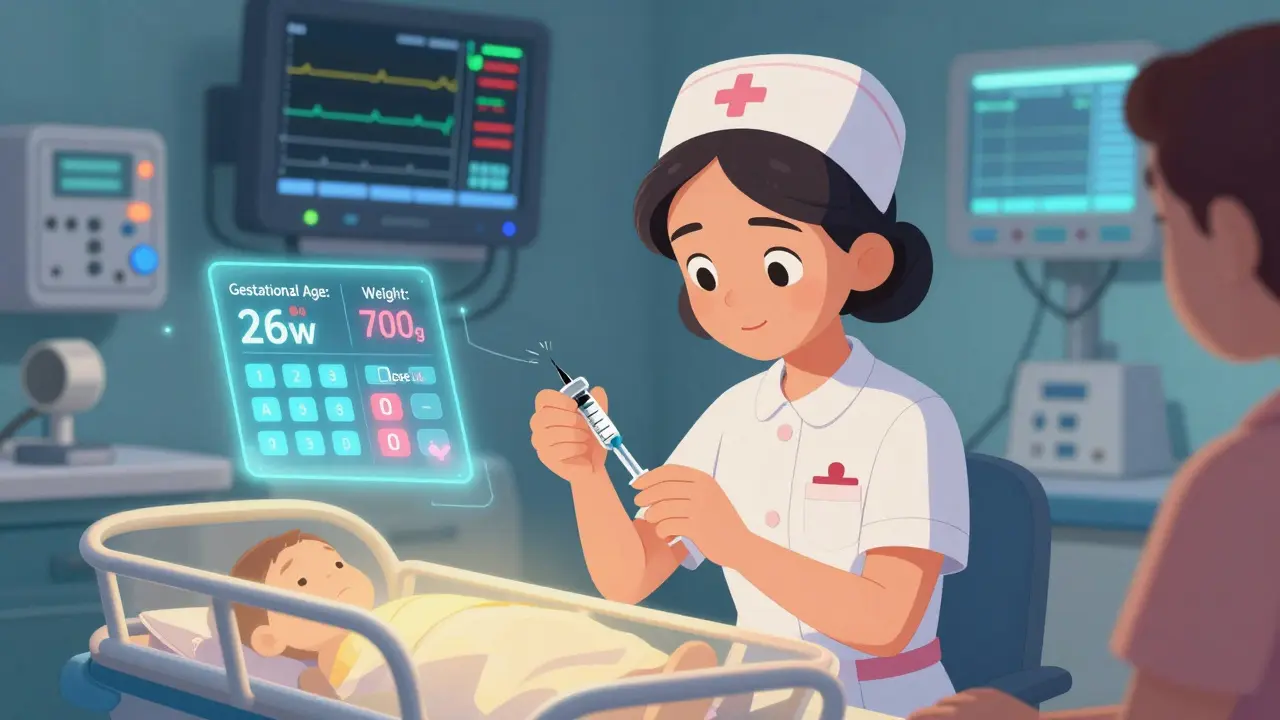
Preterm Infant Dosing Calculator
Adjust Medication for Preterm Infants
Calculate safe dosages based on gestational age and weight. The article explains that preterm infants have underdeveloped organs and require special dosing considerations.
When a baby is born too early, their body isn’t ready for the world-or for the drugs they might need to survive. Preterm infants, especially those born before 28 weeks, face a harsh reality: they’re more likely to need life-saving medications, but their underdeveloped organs can’t handle them the way older babies or adults can. What seems like a simple dose of painkiller or antibiotic can have lasting consequences. This isn’t just about short-term side effects. It’s about how these drugs change brain development, gut health, and even long-term immunity.
Why Preterm Infants Are So Sensitive to Medications
It’s not just that preterm babies are small. Their bodies work differently. Drug absorption, distribution, metabolism, and elimination all depend on organ maturity-and in a baby born at 26 weeks, those systems are barely functional. The liver, which breaks down most drugs, is still learning how to do its job. Kidneys that filter waste are still developing. Blood vessels are leaky. Even body fat, which helps store some medications, is nearly absent.
Take caffeine citrate, one of the most common drugs given to preterm infants for apnea. It’s effective-but not harmless. About 1 in 5 babies on standard doses develop a racing heart, and nearly 1 in 14 have trouble feeding. These aren’t rare side effects. They’re expected outcomes in a population where normal adult dosing guidelines don’t apply.
And it gets worse. At 32 weeks’ gestation, the enzymes that break down drugs like morphine or fentanyl are only 30% as active as they are in adults. That means a drug given to a 32-week-old baby might stay in their system twice as long as it would in a full-term infant. Dosing isn’t just about weight-it’s about gestational age, postnatal age, and whether the baby has a patent ductus arteriosus (PDA). Babies with PDA can have up to 80% more volume of distribution for some drugs, meaning the same dose can have wildly different effects.
The Hidden Cost of Routine Medications
For years, NICUs gave sedatives and painkillers like opioids and benzodiazepines as a matter of course. It was thought that preterm infants didn’t feel pain the same way. We now know that’s false. They feel pain more intensely. But here’s the twist: treating that pain with drugs can cause more harm than the pain itself.
Research published in JAMA Network Open in 2021 found that 100% of extremely preterm infants received some form of analgesia or sedation during their NICU stay. Nearly half got opioids. Nearly a third got benzodiazepines. These drugs aren’t harmless. They can disrupt brain development, delay motor skills, and increase the risk of long-term cognitive delays. And yet, the AAP now advises against routine use of these drugs-not because pain isn’t real, but because the tools we use to manage it are too blunt.
Anti-reflux medications are another example. Proton pump inhibitors (PPIs) like omeprazole are given to nearly 4 in 10 preterm infants. Why? Because they’re fussy, spit up a lot, or seem uncomfortable. But multiple studies now show these drugs don’t help. In fact, they increase the risk of necrotizing enterocolitis (NEC) by 1.67 times, late-onset sepsis by nearly 2 times, and bone fractures by 2.3 times. The 2024 AAP update now explicitly recommends against using them unless there’s a clear, proven indication.
Antibiotics: A Necessary Evil with Lasting Damage
Antibiotics are lifesavers-but they also wreck the gut. Preterm infants are often given antibiotics for suspected infections, even when there’s no proof of infection. In one study, 47% more harmful bacteria like Enterobacteriaceae were found in the guts of preterm infants exposed to antibiotics. Beneficial bacteria like Bifidobacterium dropped by 32%. And the damage didn’t go away. These changes persisted for 18 months after discharge.
Worse, antibiotic-resistant genes increased 2.8 times. That means even after the infection is gone, the baby’s gut is now a breeding ground for superbugs. Dr. Gautam Dantas from Washington University puts it plainly: "The makeup of your gut microbiome is pretty much set by age 3, and then it stays pretty stable." What happens in the NICU can shape a child’s immune system for life.
One parent on Reddit shared: "My son received 28 days of antibiotics for possible sepsis that was never confirmed. Now at age 2, he’s had five ear infections and two rounds of antibiotics." This isn’t an outlier. It’s a pattern.
Medication Errors Are More Common Than You Think
Most NICU medications are given based on weight. But weighing a 700-gram baby accurately isn’t easy. Nurses report that 68.4% encounter at least one dosing error per month. Of those, 23.7% lead to adverse events-like a baby going into cardiac arrest from an overdose of dopamine, or a seizure from too much phenobarbital.
Even small mistakes matter. A 0.1 mL error in a 1.2 kg infant is a 10% overdose. That’s not a typo. That’s a life-altering event. And it’s not always the nurse’s fault. Many medications don’t come in infant-appropriate formulations. Pharmacists have to dilute adult vials, draw up tiny volumes with syringes, and hope for precision. No wonder 76.3% of NICU medication protocols require modifications based on gestational age.
What’s Changing-and What’s Working
Change is happening. NICUs that use standardized weaning protocols for opioids and sedatives cut medication exposure by over 14 days without increasing pain scores. That’s huge. It means we can keep babies comfortable without poisoning them.
Some hospitals now use pharmacokinetic modeling software like DoseMeRx. It’s not magic-but it helps. In infants under 28 weeks, it reduced dosing errors by nearly 60%. That’s not a small win. It’s a game-changer.
And there’s hope on the horizon. The FDA has Fast-Track status for a new fentanyl formulation made specifically for preterm infants (NeoFen). Clinical trials are underway for antibiotics that spare the gut microbiome. The Neonatal Precision Medicine Initiative is building gestational age-specific models for 25 high-risk drugs by 2026. These aren’t theoretical ideas. They’re real, active projects.

What Parents and Providers Should Ask
If your baby is in the NICU, here are five questions to ask:
- Is this medication FDA-approved for preterm infants? If not, why are we using it?
- Has the dose been adjusted for my baby’s gestational age, not just weight?
- Is there evidence this drug actually helps, or are we just doing it "because we always have"?
- Are we monitoring for side effects like tachycardia, feeding intolerance, or signs of infection?
- Can we reduce or stop this drug sooner than planned?
Parents aren’t expected to be pharmacologists. But they are their baby’s best advocates. If a drug is given without clear benefit-and with known risks-it’s worth asking why.
The Bigger Picture
Preterm birth affects 1 in 10 babies in the U.S. Each year, medication-related complications contribute to 18.3% of neurodevelopmental impairments in these infants. That’s over $2.4 billion in extra healthcare costs by age 5.
We can’t stop preterm birth. But we can stop giving drugs blindly. We have the science. We have the tools. What we need is the will to change.
The future of neonatal care isn’t about giving more drugs. It’s about giving the right drugs, at the right time, in the right dose-and knowing when not to give anything at all.







so i read this whole thing and honestly? i didn't know half this stuff. like, i thought NICU meds were just... standard. turns out they're basically guesswork with a syringe. wild.
You know what really gets me? It’s not that the science is missing-it’s that the systems aren’t built to handle it. We’ve got pharmacokinetic models that can predict drug behavior in preemies down to the milliliter, but hospitals still rely on nurses eyeballing diluted adult vials because the FDA hasn’t approved infant-specific formulations. It’s not negligence. It’s inertia. And inertia kills. I’ve seen it. I’ve worked in NICUs. The weight-based dosing? It’s a joke. A 0.1 mL error in a 700g infant? That’s not a typo. That’s a near-death event. And we act like it’s just part of the job. We need to stop normalizing this.
The PPI data is terrifying. I work in neonatal pharmacology and we’ve been pushing back on routine omeprazole for years. The gut microbiome disruption alone should’ve been a red flag. But hospitals keep prescribing it because parents panic when their baby spits up. We’re treating symptoms, not causes. And honestly? The AAP’s 2024 update is a win, but it’s too little, too late for so many kids already damaged.
ok but like... who gave doctors the right to experiment on babies? this is just pharma lobbying disguised as medicine. they don't care about the kids. they care about the next patent. antibiotics? sedatives? all profit centers. and the parents? they're just scared and told to 'trust the system'. lol.
I just want to say thank you to every NICU nurse reading this. You’re doing the impossible with broken tools. I’ve got a 2-year-old who spent 47 days in the NICU, and I never realized how much pressure you’re under-dosing by guesswork, no proper formulations, parents begging for ‘something’ to fix everything. You’re not just saving lives. You’re holding back chaos. I see you. And I’m so grateful.
This article is an indictment of modern American medicine. We have abandoned the Hippocratic Oath in favor of bureaucratic convenience. Medicating preterm infants without FDA approval? This is not healthcare. This is corporate negligence. The fact that we allow such practices to continue is a moral failure of the highest order. The Founding Fathers would weep.
i mean... if the drugs are so dangerous, why are they even used? maybe we should just... not give them? sounds simple. why overcomplicate it?
let me guess... the FDA is in bed with Big Pharma. they’re the ones blocking infant-specific formulations. why? because if they approved real pediatric dosing, they’d have to audit every hospital. and nobody wants that. this whole thing is a cover-up. mark my words: the next pandemic will come from antibiotic-resistant preemies. and they’ll blame the parents.
i just had a preemie. we were given morphine for 11 days. no one told us about the long-term risks. i didn’t even know to ask. this article should be mandatory reading for every NICU parent.
The fact that we’re even having this conversation is progress. I’ve seen NICUs shift from ‘drug first’ to ‘assess first’-and the outcomes are better. Less sedation. Fewer infections. Happier babies. It’s not about doing nothing. It’s about doing smarter. And honestly? That’s the future.
In India we have same problem but worse. No monitoring. No protocols. Just weight-based dosing from adult vials. We use 1/10th of a syringe for 800g babies. No one has training. No one has time. We pray. And sometimes, the baby lives. Sometimes not. This article? It’s not just American. It’s global. We need global standards. Not just in the U.S. We need it everywhere.