Bladder Spasms: Causes, Symptoms and What Helps
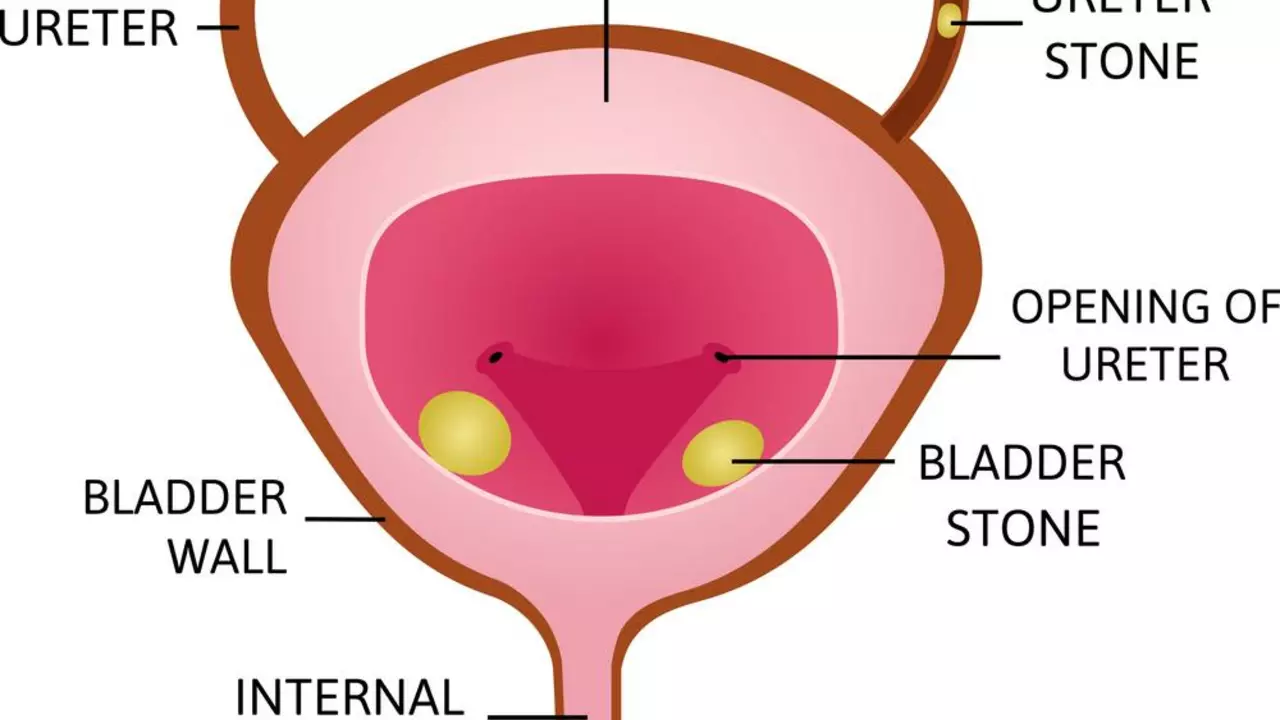
Bladder spasms can feel sudden and scary — a sharp urge to go, cramps low in the belly, or leaks you didn't expect. They're common and can come from many causes: infections, nerve problems, bladder stones, certain meds, or after surgery. Knowing the likely cause helps you get the right treatment fast.
When a spasm hits, the detrusor muscle in the bladder contracts too often or too hard. That drives urgent trips to the toilet and sometimes incontinence. People with overactive bladder, urinary tract infections (UTIs), multiple sclerosis, spinal injuries, or diabetes can have spasms more often. Even stress, caffeine, alcohol, and spicy foods can make them worse.
How to spot bladder spasms
Watch for an intense, sudden need to urinate, frequent bathroom trips, nighttime urination, cramping in the lower belly, or accidental leaks. Pain with urination or cloudy, strong-smelling urine suggests a UTI and needs prompt testing. If you suddenly can't pass urine or have fever and severe pain, get urgent care.
Simple steps that help right away
Start with small, practical fixes at home. Cut back on caffeine, alcohol, and acidic drinks. Try timed voiding — schedule bathroom breaks every 2–4 hours to retrain the bladder. Pelvic floor exercises (Kegels) can calm spasms by giving better control. Use a heating pad on the lower belly for short-term relief.
Medically, doctors may prescribe antimuscarinic drugs or beta-3 agonists to relax the bladder muscle. If a UTI is the cause, antibiotics clear the infection and often stop spasms. For nerve-related spasms, treatments include Botox injections to the bladder or nerve stimulation therapies. Surgery is rarely needed but may be an option when other treatments fail.
Keep a bladder diary for a few days: note fluids, bathroom times, leakage, and triggers. That helps your clinician see patterns and pick the right treatment faster. Bring a list of current medicines too — some drugs cause urinary urgency or retention.
If you live with chronic bladder spasms, combine medical care with lifestyle moves: weight loss if needed, smoking cessation, pelvic health physiotherapy, and managing constipation. Mindfulness and breathing can reduce the reflex that worsens urgency in stressful moments.
Also, track patterns around sex, exercise, and weather — some people notice spasms flare with sexual activity, heavy lifting, or cold exposure. Sharing those patterns with your clinician helps pinpoint triggers. Patient forums and pelvic health clinics can offer practical tips and support for coping.
When to see a doctor? If symptoms start suddenly, if you have fever or back pain, if you can't urinate, or if symptoms affect daily life, see a healthcare provider. They will likely do a urine test, check for post-void residual urine, and sometimes order imaging or nerve tests.
Bladder spasms are treatable. With the right steps — simple lifestyle changes, targeted meds, or specialized procedures — most people get clear improvement. Keep track of your symptoms and work with a clinician to find the combination that helps you live without constant urgency.