Liquid Medication: How It Works, Who Uses It, and What You Need to Know
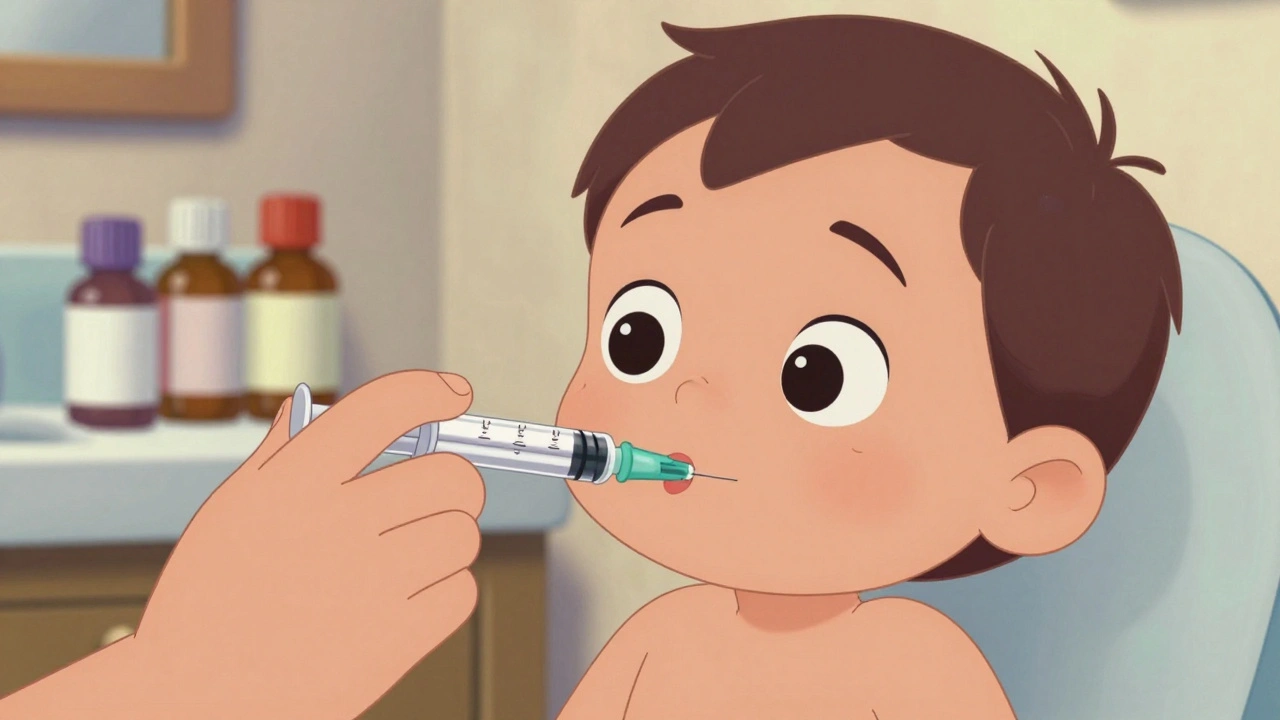
When you need medicine but can’t swallow pills, liquid medication, a form of drug delivered in solution or suspension for easier ingestion. Also known as oral liquids, it’s often the only option for children, older adults, or anyone with swallowing difficulties. It’s not just a softer version of a pill—it’s a different way of delivering treatment, with its own rules for accuracy, storage, and timing.
Liquid medication is common in pediatric meds, formulations designed specifically for infants and young children, where precise dosing based on weight is critical. It’s also used in medication adherence, the practice of taking drugs exactly as prescribed for seniors with memory issues, because liquids can be easier to track and mix with food or drinks. But here’s the catch: measuring liquid correctly matters more than you think. A teaspoon from your kitchen isn’t the same as the dosing cup that comes with the bottle. One wrong measurement can mean too little effect—or too much risk.
Many people assume liquid meds are just easier versions of pills, but they often have different active ingredients, concentrations, or even additives like sugar or alcohol. That’s why checking the drug formulary, a list of medications approved and covered by your insurance plan is essential. Some insurance plans don’t cover certain liquid forms unless the pill version fails first. And if you’re switching from a tablet to a liquid, your doctor might need to adjust the dose—because the body absorbs liquids differently.
For parents, caregivers, or anyone managing meds for someone else, liquid medication brings both freedom and responsibility. You can crush a pill and mix it with applesauce, but you can’t always do the same with a liquid. Some suspensions need shaking before each use. Others must be refrigerated. Some lose potency after 14 days. Ignoring those details isn’t just inconvenient—it’s dangerous.
And it’s not just about kids or seniors. People with chronic conditions like epilepsy, Parkinson’s, or severe nausea often rely on liquid forms to stay on track. Even when you’re feeling fine, consistency matters. That’s why so many of the posts below focus on how to make liquid meds work in real life—how to time doses while breastfeeding, how to avoid interactions with food or other drugs, and how to store them safely without wasting money.
Below, you’ll find real-world advice from people who’ve been there: how to measure accurately, how to talk to your pharmacist about alternatives, how to handle missed doses, and how to spot when a liquid isn’t working like it should. Whether you’re giving medicine to a child, managing your own treatment, or helping an aging parent, the right liquid medication can make all the difference—if you know how to use it right.