Polymyositis: what it is and what to watch for
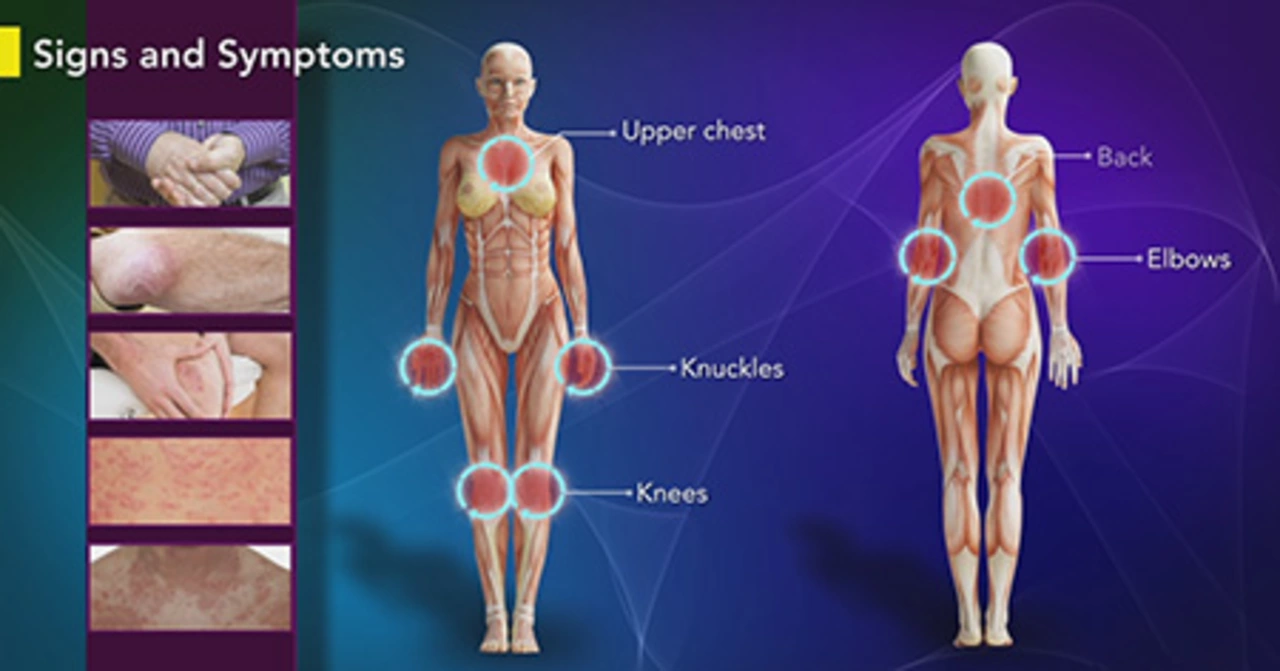
Polymyositis is an inflammatory muscle disease that slowly weakens muscles, usually in the shoulders, hips, and neck. It’s not common, but when it shows up you’ll often notice trouble rising from a chair, climbing stairs, or lifting your arms. That gradual weakness, plus muscle aches and sometimes tiredness, is what usually sends people to their doctor.
How doctors diagnose polymyositis
Diagnosis is a step-by-step process. Your doctor will combine a medical history and a physical exam with simple tests: blood work for muscle enzymes (like CK), autoimmune antibodies, and often an EMG (electrical test of muscle). Imaging such as MRI can show inflammation, and a muscle biopsy sometimes confirms the diagnosis. These tests help rule out other causes like thyroid disease, infections, or drug-related muscle problems.
If you have persistent, symmetric muscle weakness (both sides of the body) and raised muscle enzymes, ask your doctor about an EMG and MRI. If results are unclear, a biopsy is the next step; it gives the clearest picture of muscle inflammation.
Treatment choices: what to expect
First-line therapy usually starts with corticosteroids such as prednisone to reduce inflammation quickly. Many people respond well, but long-term steroid use can cause side effects. That’s why doctors often add steroid-sparing drugs—medications that let you lower the steroid dose. Typical options include azathioprine and mycophenolate, and newer choices like JAK inhibitors are showing promise for certain patients.
Medication is only one part of care. Physical therapy helps keep muscles flexible and rebuild strength without overdoing it. Regular monitoring of muscle strength and blood tests helps tailor treatment and catch relapses early. Vaccinations and infection prevention matter, since some treatments lower immune defenses.
Wondering about online pharmacies or buying meds? Be cautious. Use licensed pharmacies and keep your prescriber involved. Our site has guides on prednisone alternatives and safe online buying—those pieces explain which drugs are commonly used and how to avoid risky sellers.
When should you see a specialist? If weakness builds over weeks to months, if swallowing or breathing gets harder, or if standard tests don’t give clear answers, ask for a referral to a rheumatologist or neuromuscular specialist. These specialists can recommend advanced tests and second-line treatments.
Living with polymyositis means balancing meds, exercise, and regular check-ins. Track your symptoms and side effects, bring notes to appointments, and don’t hesitate to ask about steroid-sparing options. If you want deeper reading, check our articles on prednisone alternatives, immune-modulating medicines, and practical tips for buying medication safely online.
If you have specific symptoms or medication questions, bring them up with your care team—this guide helps you know what to ask and what to expect next.